Clearinghouse as a commodity
A clearinghouse should function similarly to a public utility. Like utility customers, clearinghouse clients expect extremely reliable service and rapid support if there is a service outage. Clearinghouses must be able to swiftly adjust to payer related problems and communicate with clients when downtime is expected or when a problem is detected with the data provided. In all cases, changes to levels of service needs should be handled by a knowledgeable and helpful customer representative. Etactics’ IntelliClaimⓇ clearinghouse provides this level of service.
Solve common problems through claim scrubbing, eligibility verification prior to claim submission, in-portal claim editing, and workflow management.
While some practice management systems are robust and independent, others lack needed or desired functionality. In such instances, a modern clearinghouse covers the gaps between what is needed on a claim and what the HIS or PM system natively generates.
IntelliClaim offers all of the following regardless of your pricing model and practice management or hospital information system:
Claims Submission
Standard claim scrubbing such as CCI, LCD & NCD edits
Real-Time eligibility benefit verification
Real-Time claim status checks
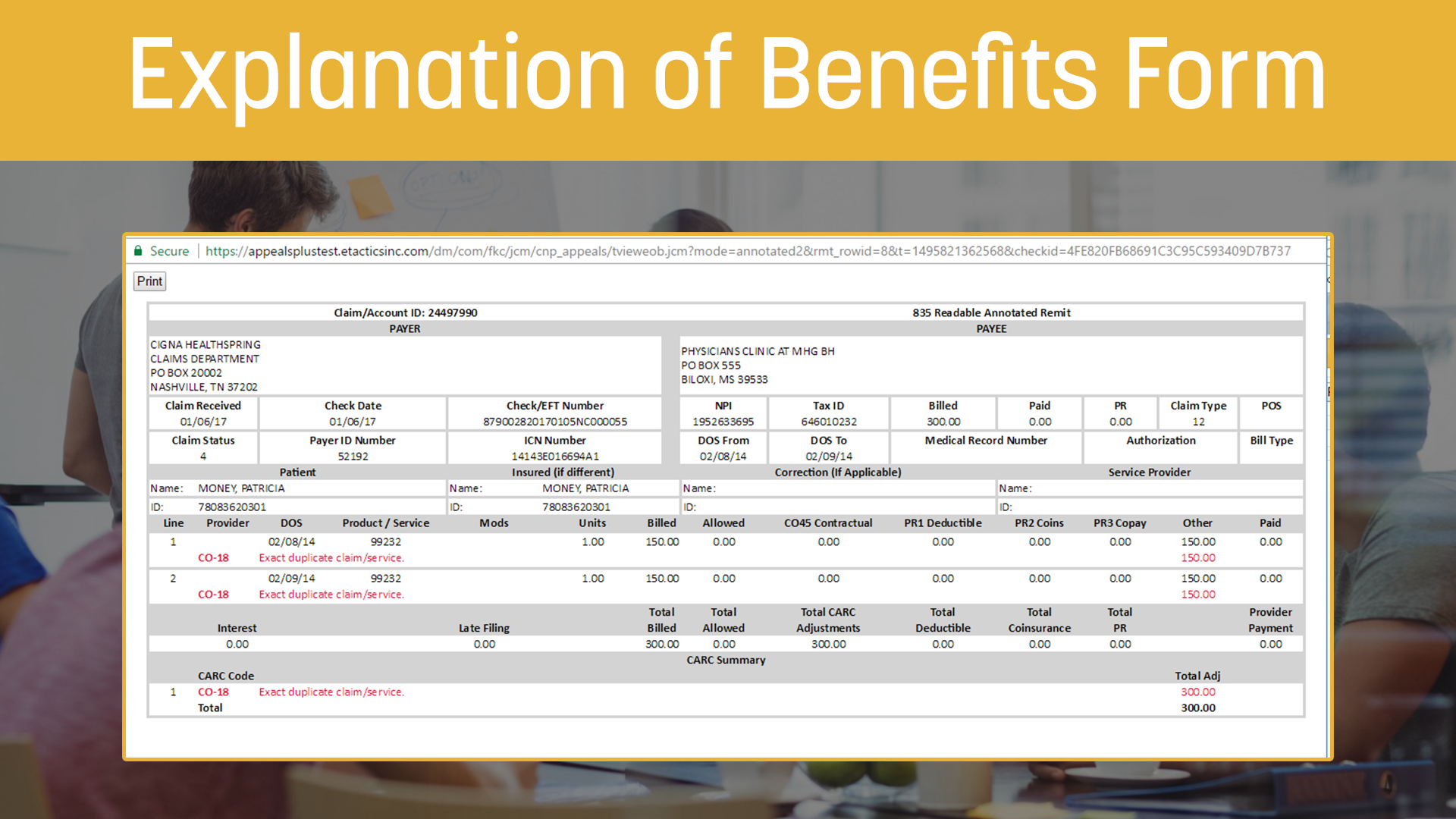
Electronic Remittance Advice (ERA) delivery
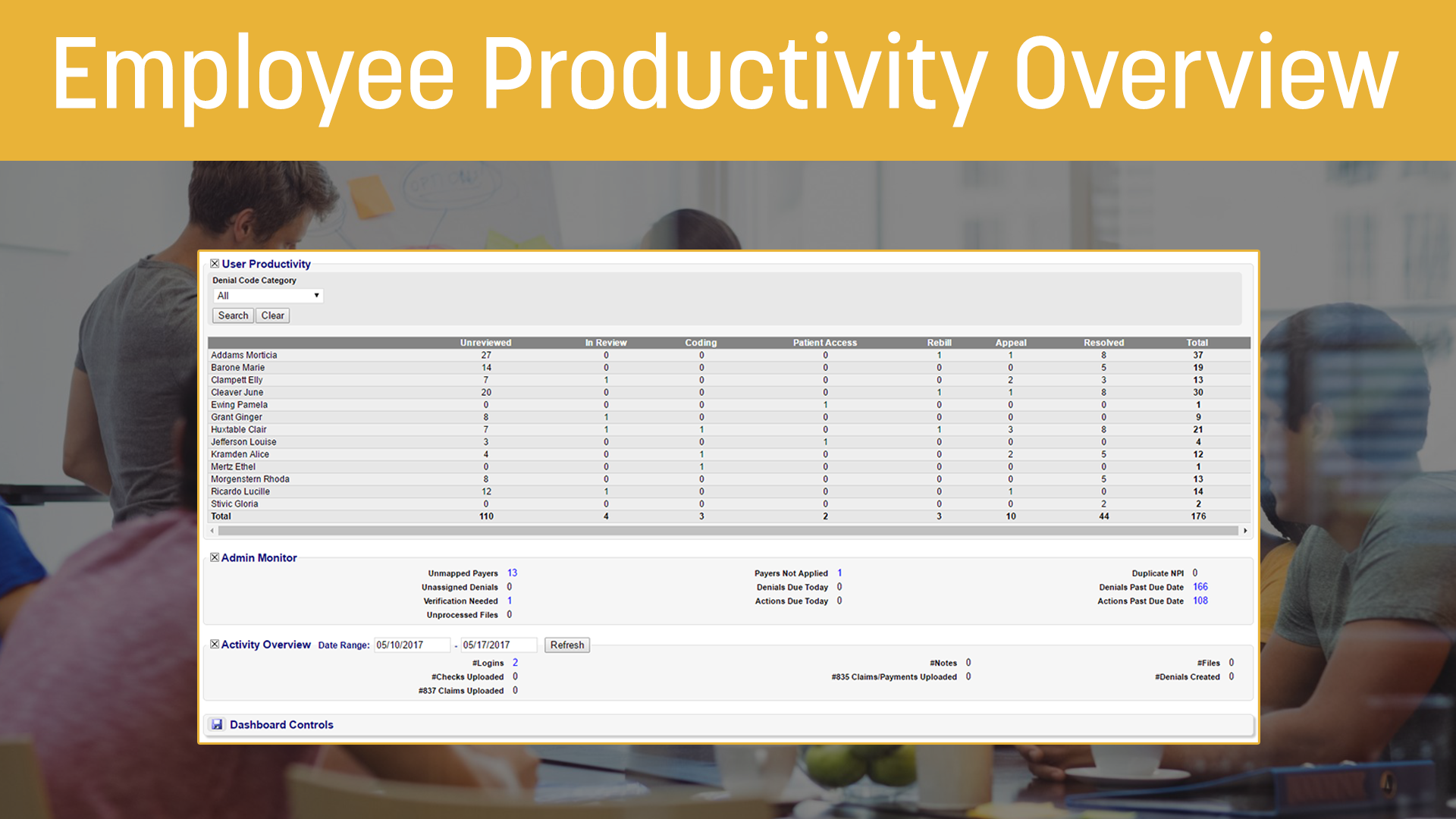
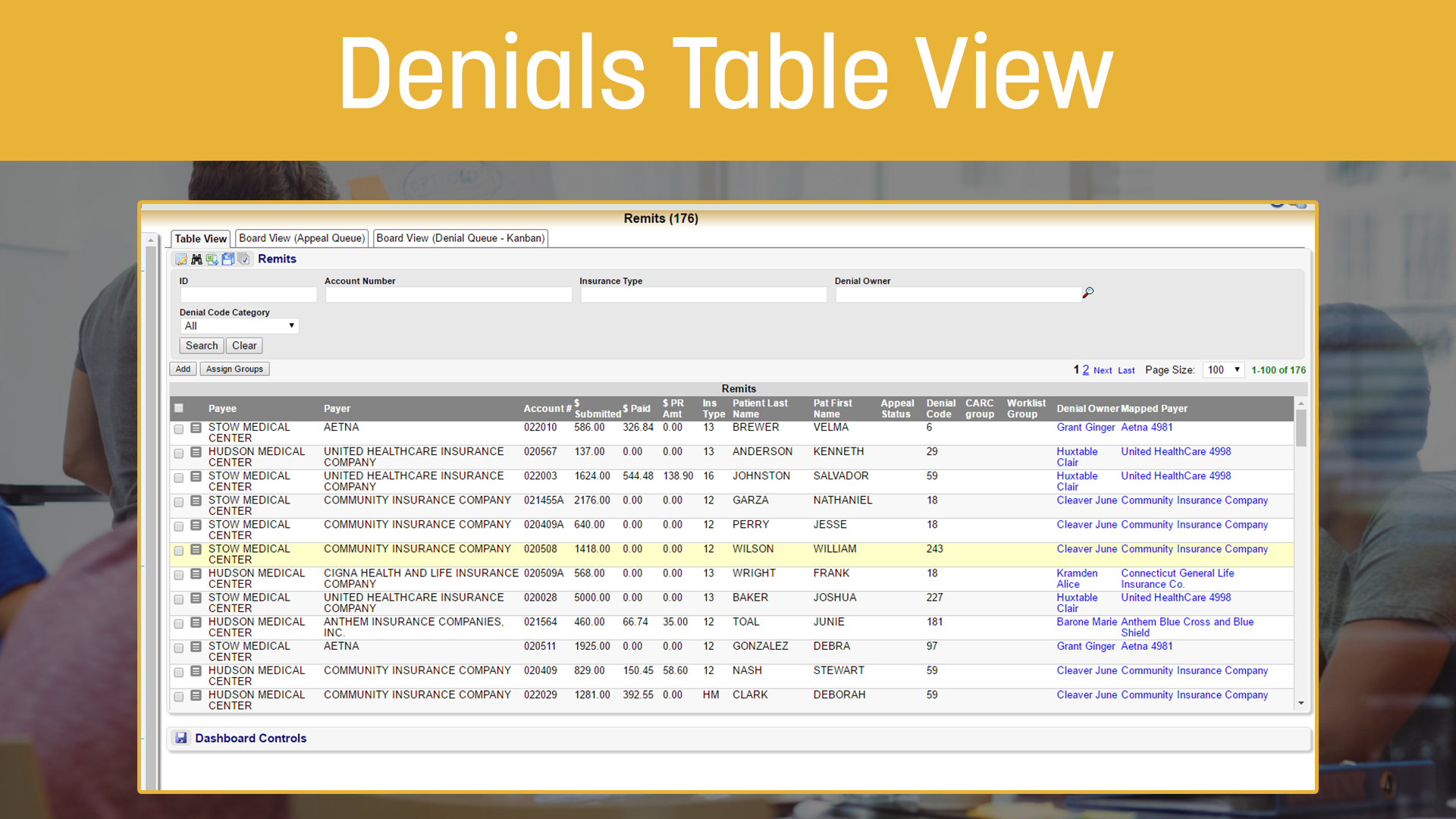
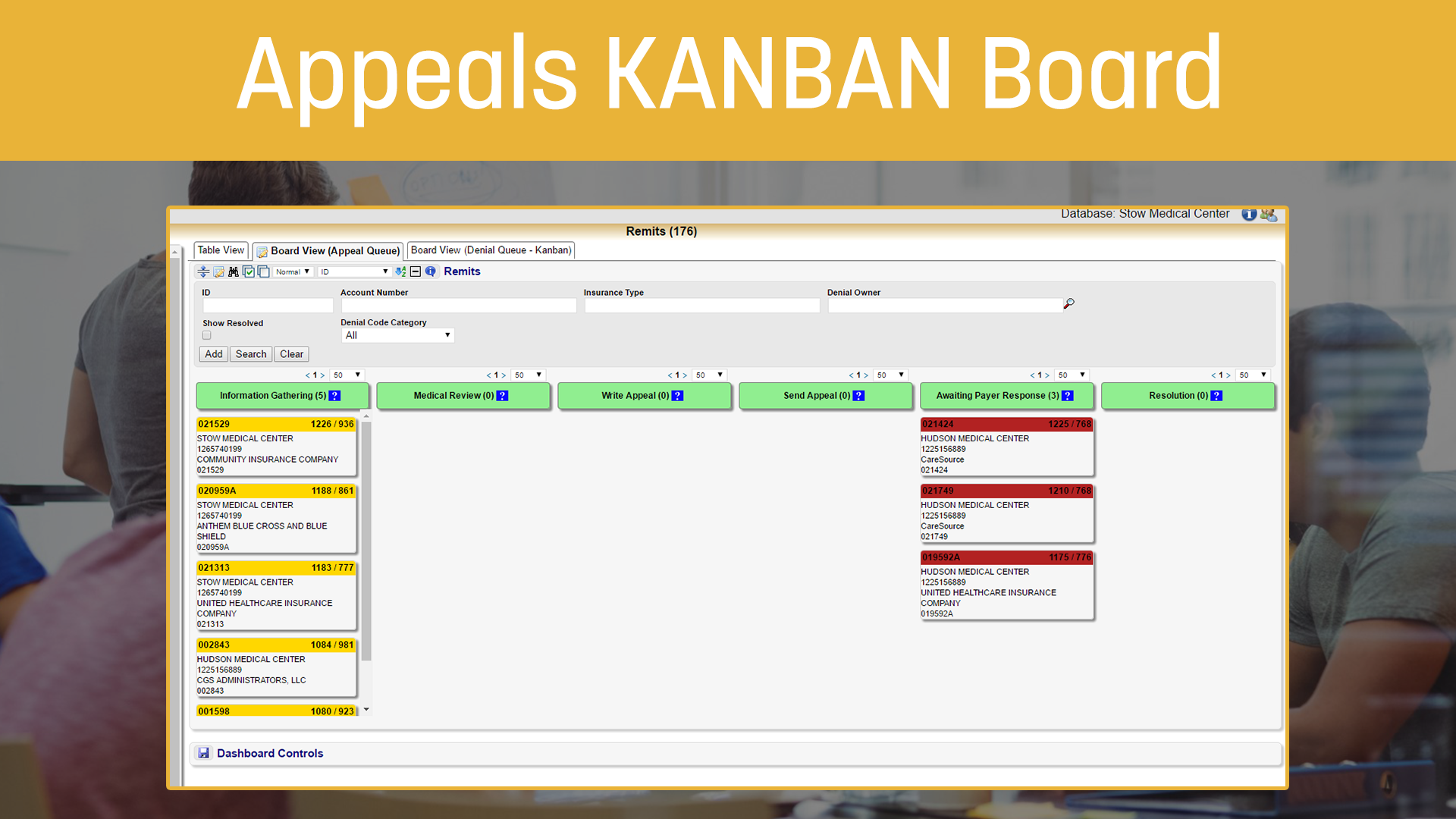
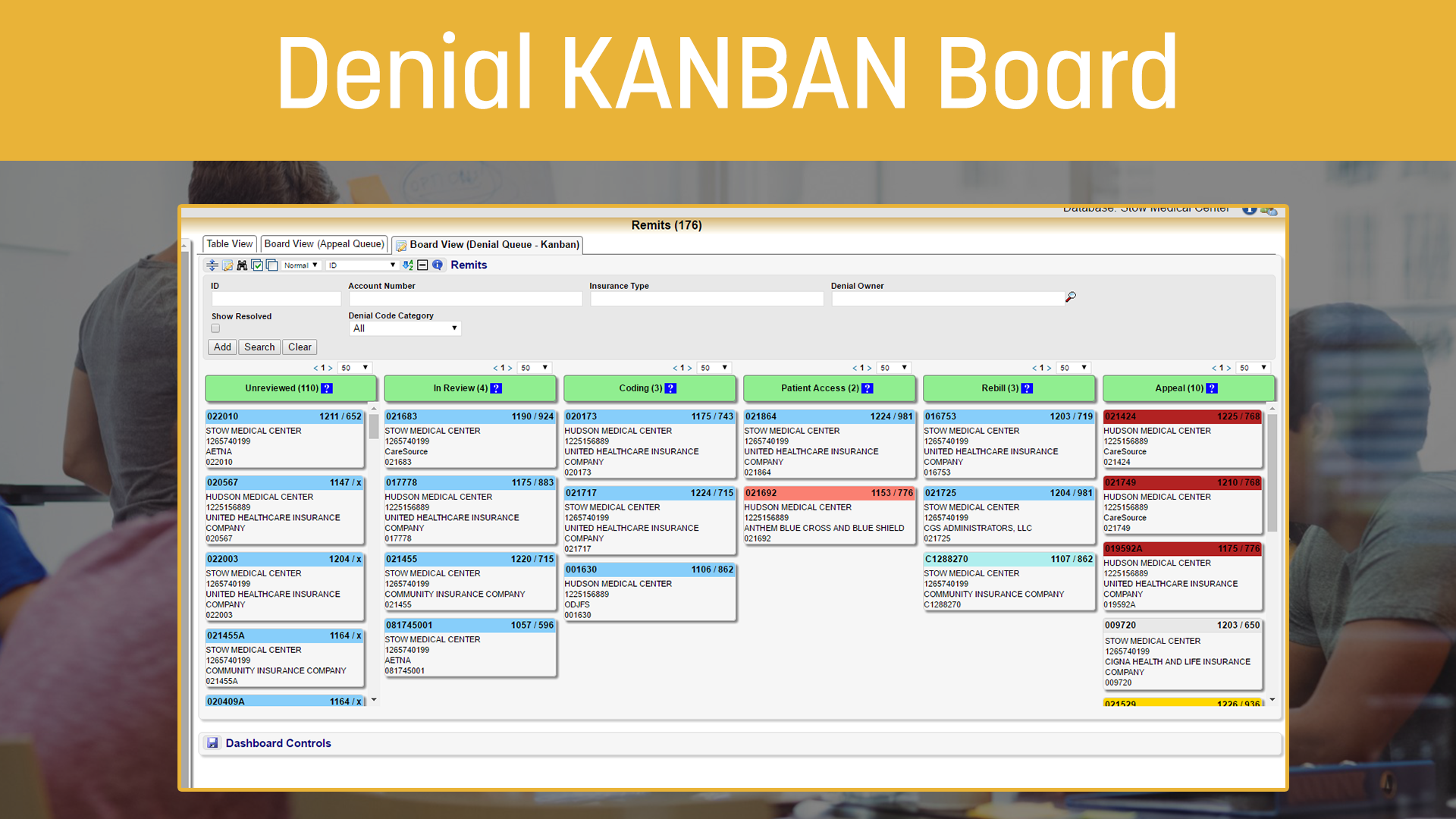
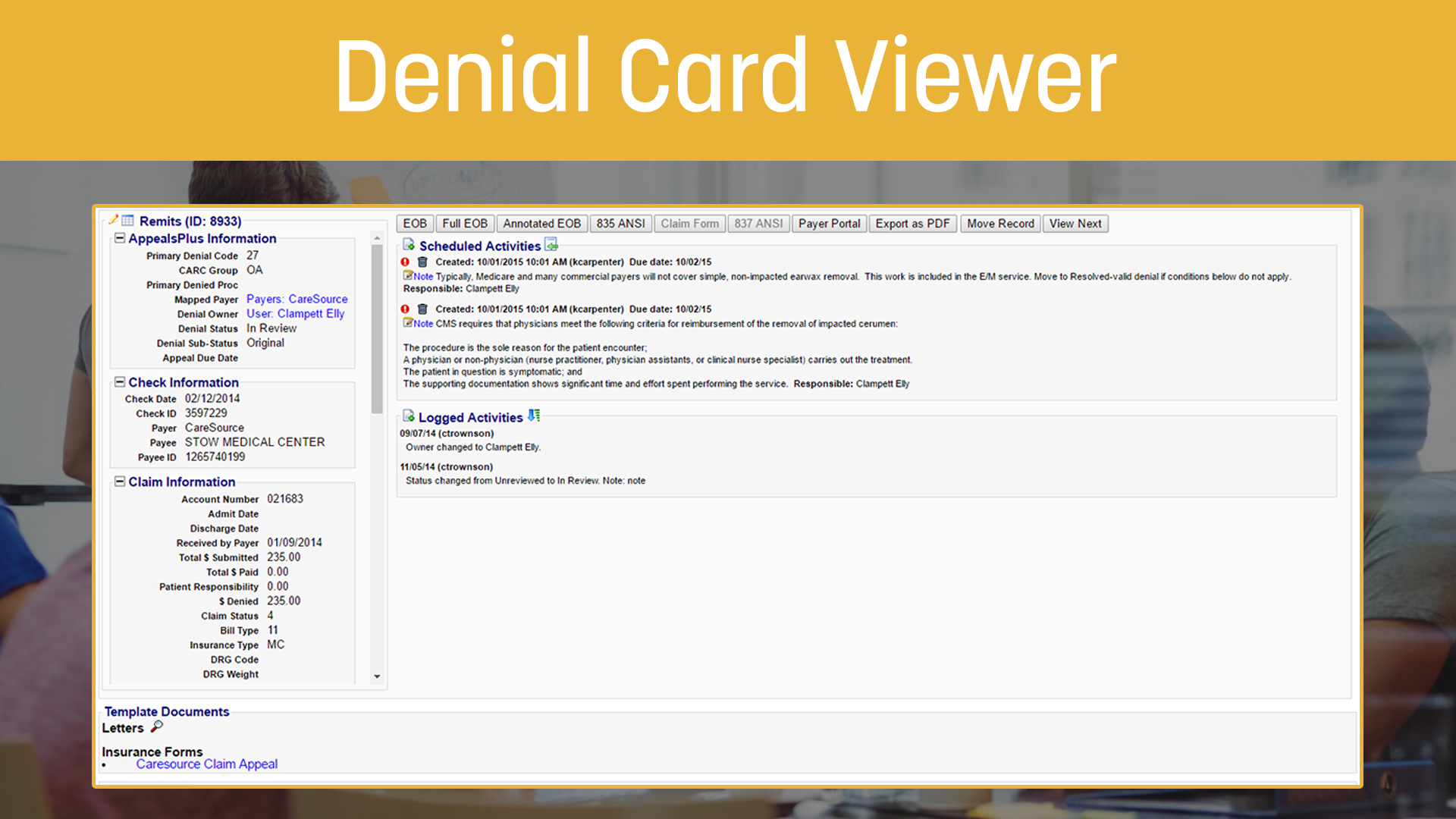
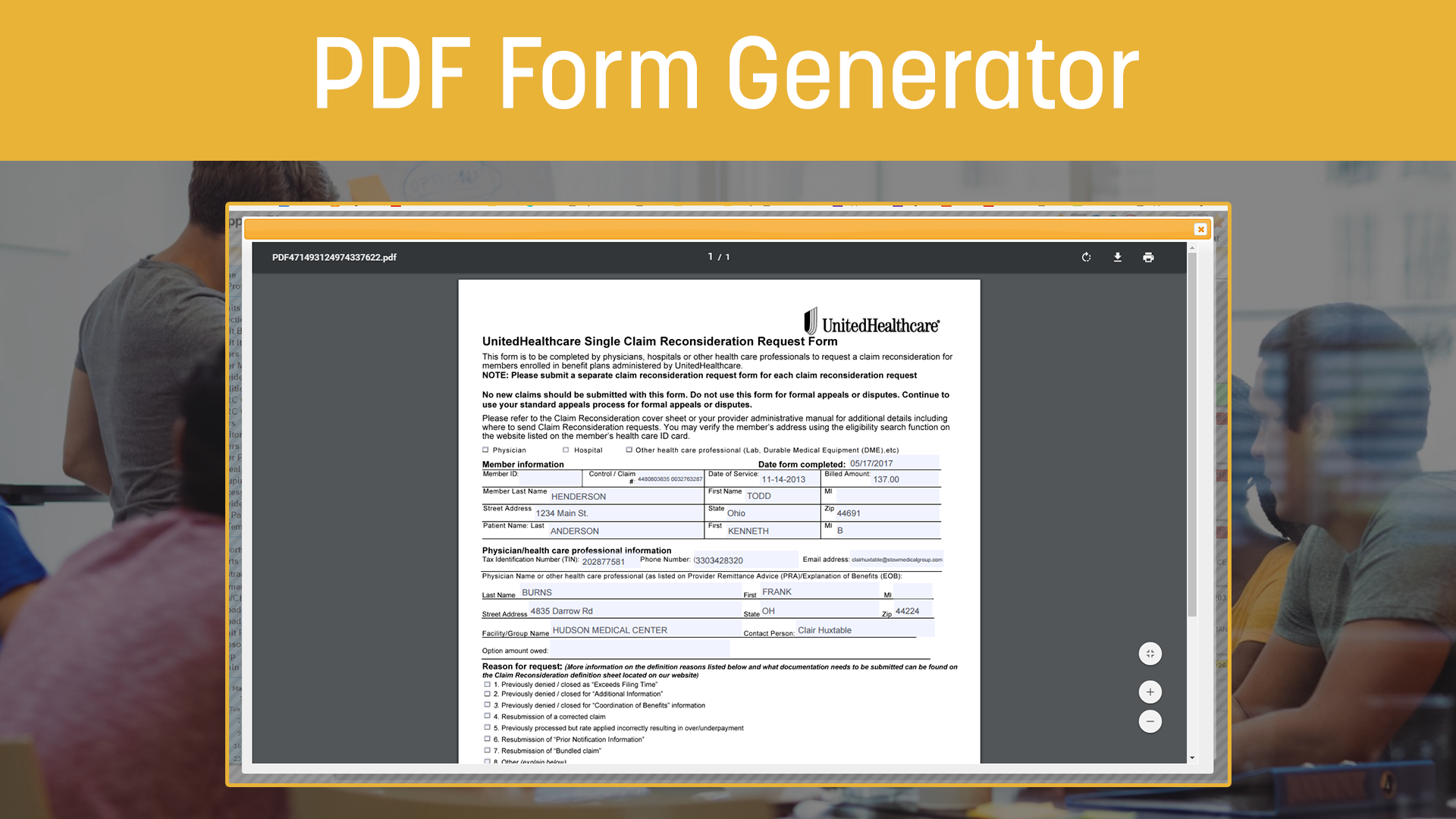
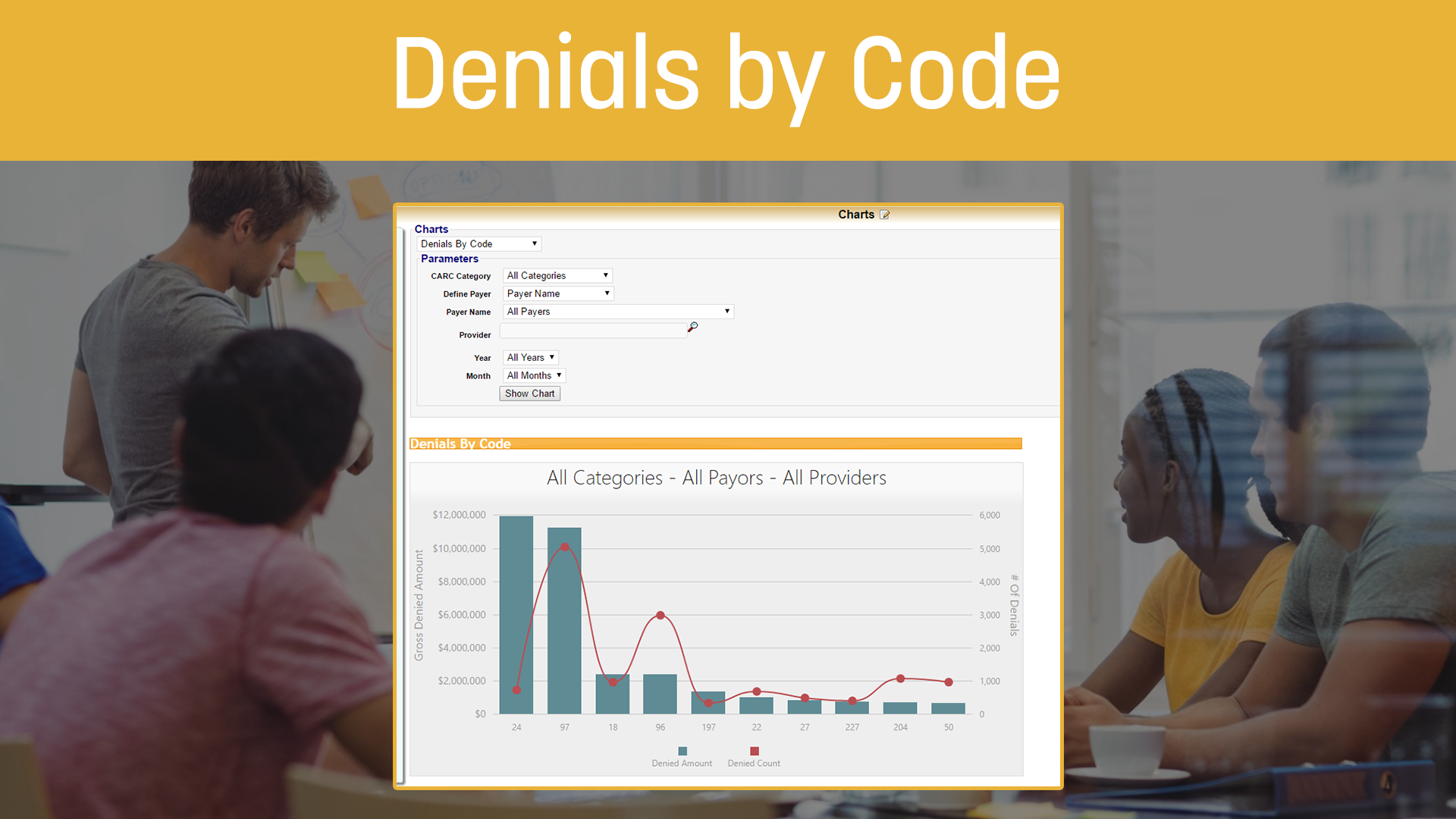
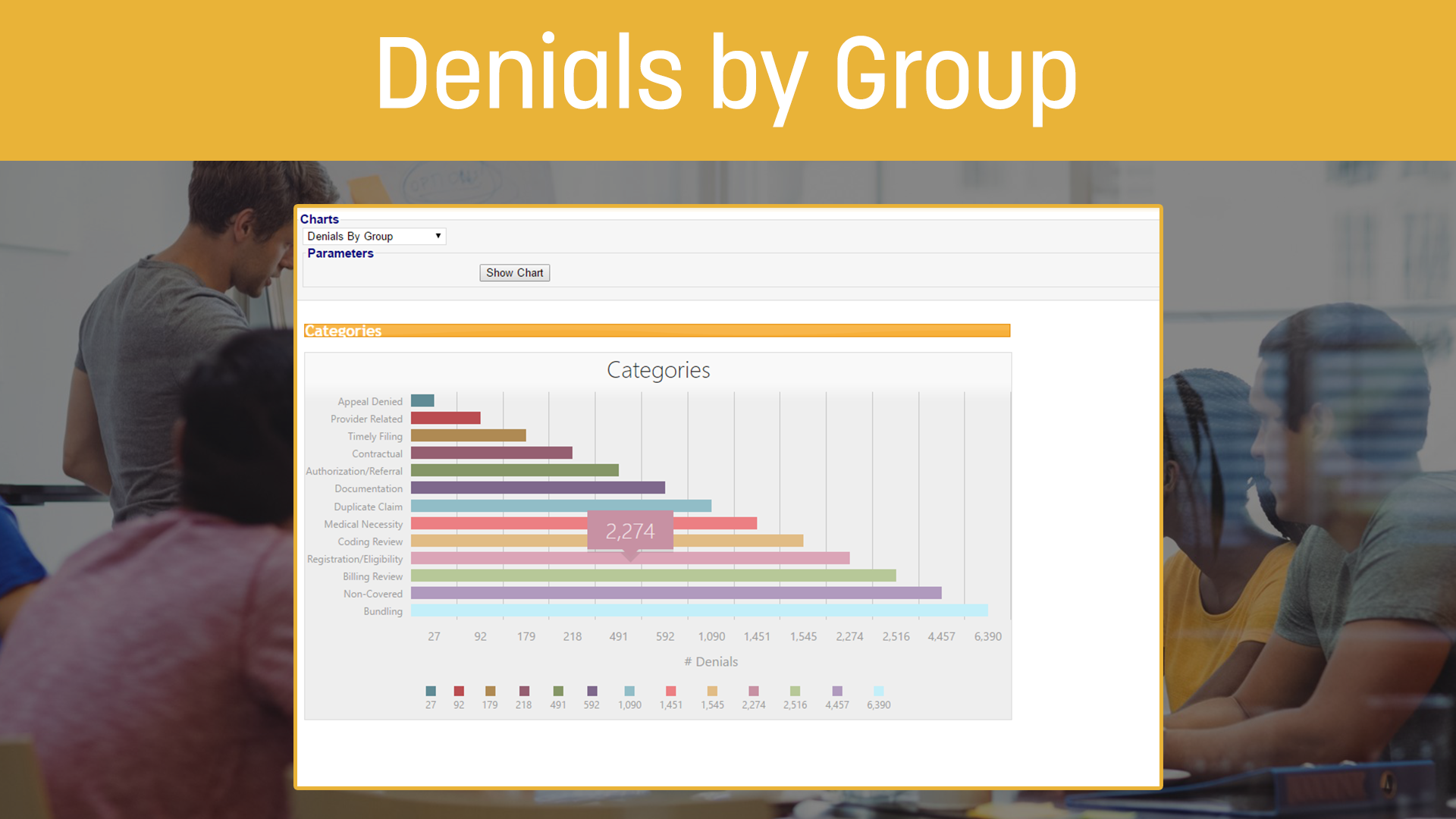
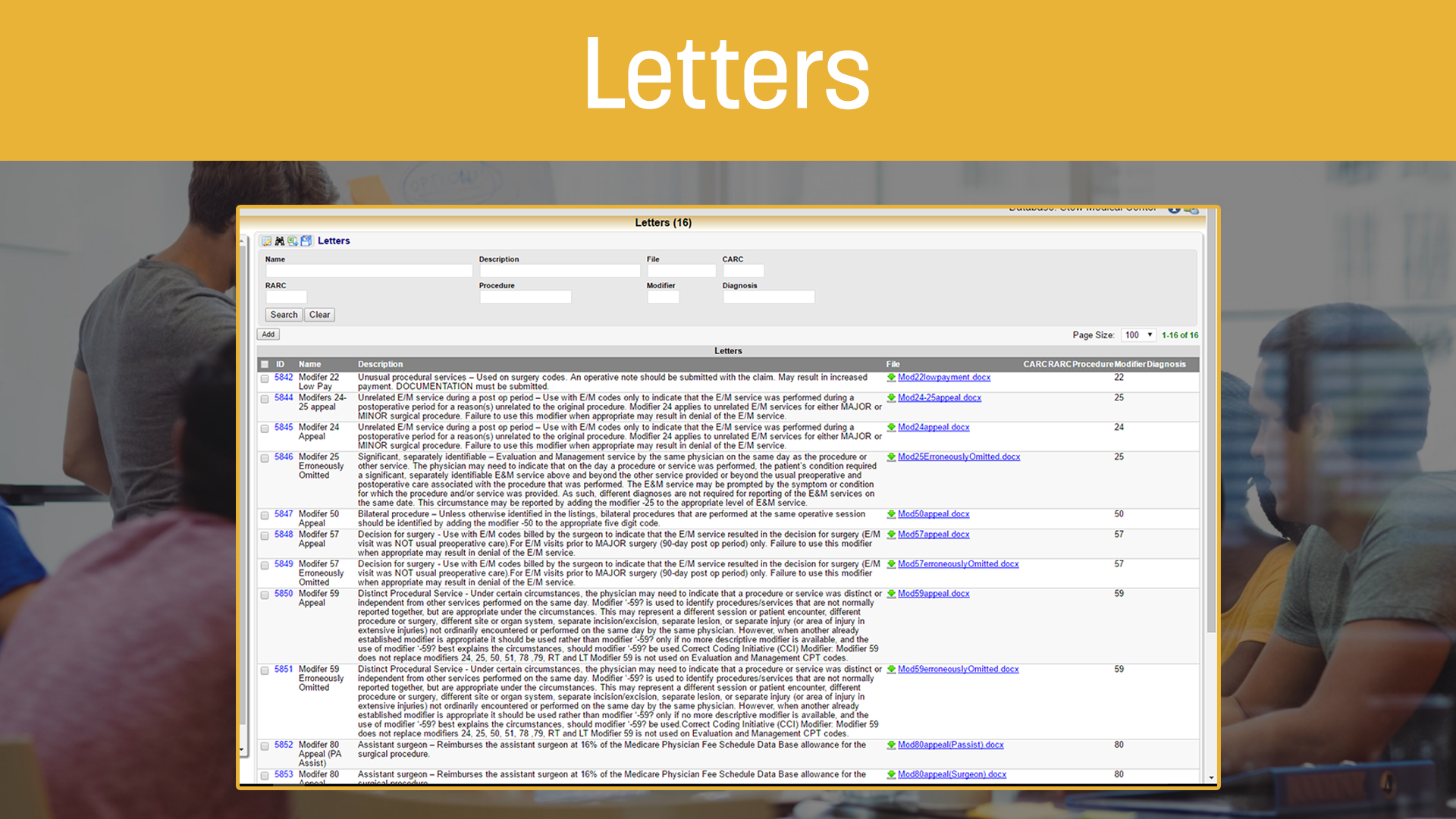
Integration to the AppealsPlus™ denial management product
Comprehensive enrollment support
World class customer service
Custom programming services to meet your unique needs
Our client managers are with you from day one including implementation and ongoing support.
We simplify and streamline the enrollment process including the verification of the receipt of ERAs and calling the appropriate payer on your behalf if there are problems.
After training, client managers are always available to answer any questions by email or phone. For more information, check out our testimonials and customer experience brochure.
Our standard claim scrubbing service applies appropriate edits to your claims, including National Coverage Decisions (NCD), Local Coverage Decisions (LCD), and Correct Coding Initiative (CCI).
Affected claims are returned to you promptly for corrective measures. These claims can be worked in our portal or from within your PM or HIS system by importing an ANSI 277CA file. Clients can also request custom edits, which can filter and highlight mistakes then place affected claims into a work queue for correction. Alternatively we will correct the claim automatically before and continue with the submission.