The American Association of Critical Care Nurses suggests that flexible visitation improves care and satisfaction. Unrestricted visitation leads to better communication, understanding of the patient, and staff satisfaction. It can also improve patient- and family-centered care.
This was especially true for people in the ICU. Out of 46 studies on patient- and family-centered care interventions, 78% had one or more positive outcomes. The length of ICU stays decreased by an average of 1.21 days.
Despite the positive effects that flexible visitation has, 90% of ICUs have restrictions for visitors. These policies also have benefits, hence why hospitals implement them in some capacity.
They serve to keep workflows functioning in a facility. Not everyone will understand the importance, so it’s necessary to create strategies that encourage following it.
Although people might think that rules are arbitrary and an inconvenience, each has significance. They balance visitation for residents’ comfort while also keeping everything running smoothly.
Purpose of Having a Policy
While flexible visitation has its benefits, it isn’t safe to have just anyone coming and going whenever they please. This poses safety, security, and health risks for hospitals.
Having a policy that limits when people come ensures that there aren’t too many people who may get in the way of care. This is especially necessary for emergency departments which typically allow fewer guests. If there are too many people, it disrupts the flow of providing treatment, especially in urgent scenarios.
Keeping track of visitors also helps protect confidentiality. With a visitor check-in policy, you can direct them to the correct room so they don’t walk into the wrong one. It also helps your staff keep track of who has consent to know the patient’s health information.
If you don’t keep tabs on who is coming in and out, it could result in a malicious person obtaining protected health information. Or worse, they could tamper with someone’s medication or treatment, resulting in serious health problems.
In 2018, a man checked into the hospital as a visitor. He injected a syringe into a patient’s IV, causing the person to go into cardiac arrest. The patient was able to identify the suspect as his roommate, but only after health workers resuscitated him.
It was good the hospital had a check-in process, but they were only able to identify him through the patient. If he had died, it would’ve been much harder to determine who the suspect was.
Better policies could have prevented this, such as requiring identification. The hospital also could’ve asked for the resident’s permission to allow this person. Without ways to regulate who is coming in, there’s no way to track who was responsible or what happened when situations like these happen.
Excess visitors contribute to other health risks with the spread of disease. The more people that enter, the more chance a guest will take germs home with them. They also could bring diseases into the hospital and pass them to vulnerable people. This makes it difficult for someone to heal from their current ailment.
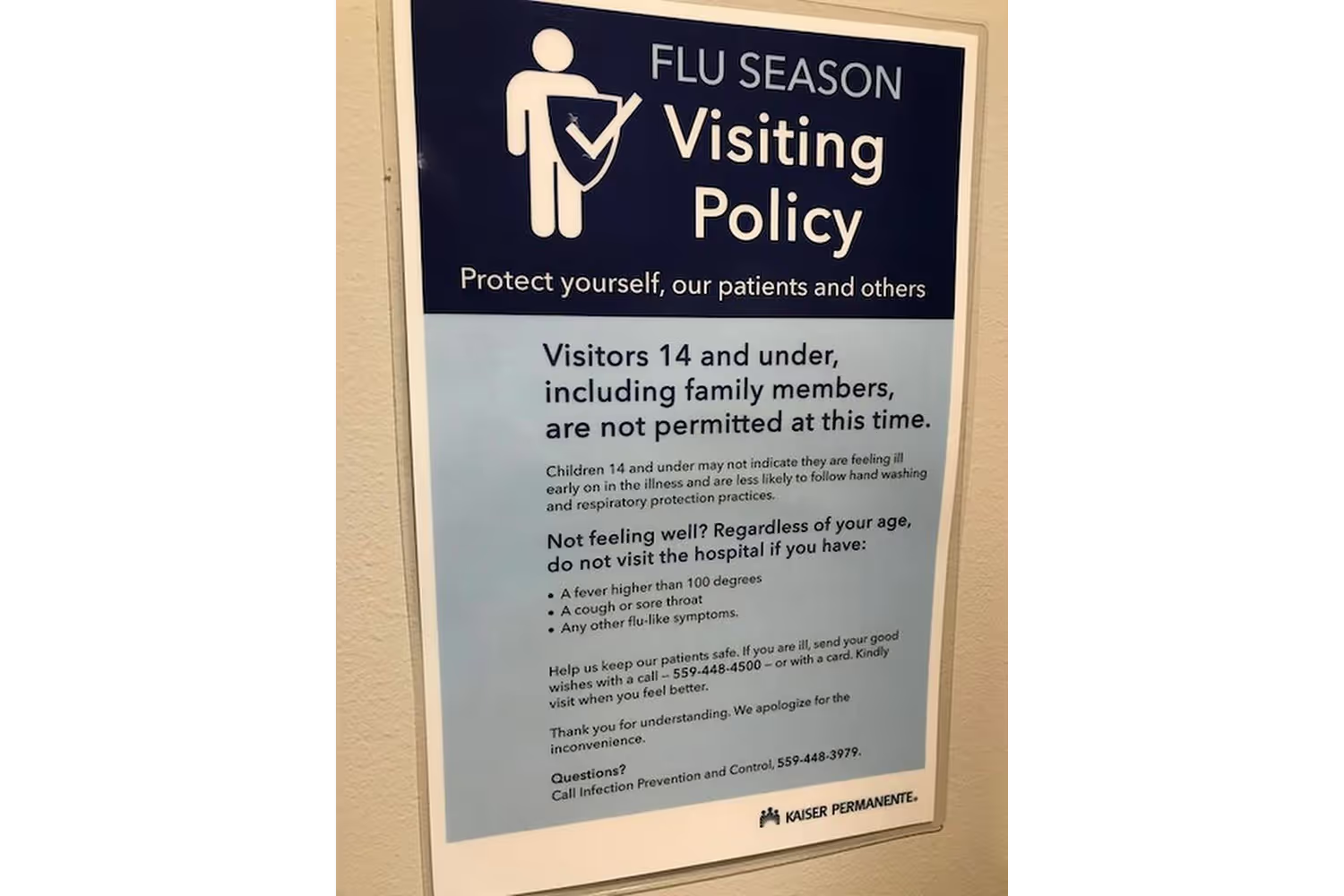
This is why during the COVID-19 pandemic, many hospitals updated their visitation policies.
The Centers for Diseases Control and Prevention advised adding limitations. Policies became more strict to prevent any possible risk for outside guests, current patients, and staff.
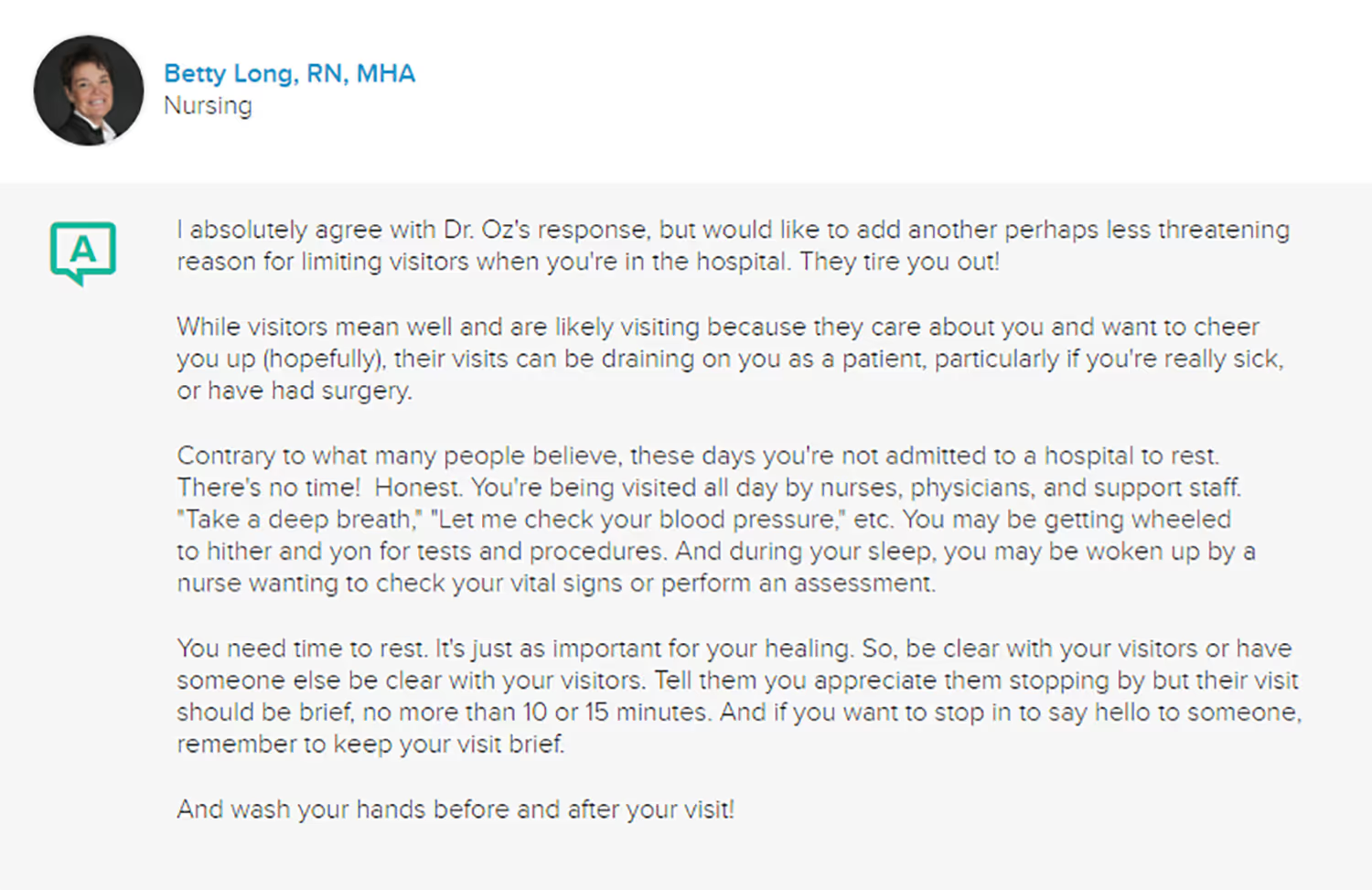
Besides health and safety, requirements also contribute to better comfort. Sure, having visitors does help people relax when they’re in the hospital. But it can also overwhelm them.
Treatments can be exhausting and sleep is so important for recovery. Sleep deprivation decreases the ability to resist bacterial and viral infections. But getting enough sleep contributes to the creation of more white blood cells that attack bacteria and viruses.
Because of this, it’s necessary to have a visitation schedule and limit how many can come at once. If they were constantly coming and going, patients would never get adequate rest.
This especially applies to semi-private rooms. For those who share, it would be disruptive to always have strangers around. You’d have a hard time relaxing too if people you didn’t know kept invading your private space while you tried to recover.
But roommates aren’t the only ones who feel uncomfortable with these visitors. Even some patients don’t want family or friends disrupting them in the hospital for the same reasons. They know their recovery is important and don’t want to deal with the interruptions.
To prevent this, some hospitals recommend for guests to check with them before coming. That way the staff can let them know if it’s a good time and if the patient would be able to enjoy the visit.
How to Get People to Follow Policies
Like anything in life, there are always people who think the rules don’t apply to them. It’s hard to explain why something is necessary when circumstances are different for everyone.
But you can’t bend the rules just because someone complains.
First, you need to educate them on what the policy is and then encourage its significance. It’s easy for guests to overlook the needs of people who they’re disrupting with frequent visits because they have good intentions.
One of the first steps is to have a check-in procedure where guests sign in at the front desk or nurse’s station within the unit. When they do this, a staff member can greet them and go over the guidelines with them so that they can’t claim that they didn’t know the policies.
Posting signs remind guests of these rules throughout their stay. It encourages them to be mindful of the other residents and also the staff’s busy schedule.
To ensure these people don’t overstay designated hours, it’s helpful to give them a heads up in advance of quiet hours. This way they don’t feel rushed out and have time to say bye to their loved ones before heading home for the day.
A final way to ensure people follow policy is to have security onsite. Now, I’m not suggesting this as a scare tactic. But this is an extra safety measure if any security concerns arise from certain guests. It’s more likely they will abide by policies if they know your practice takes it seriously.
Best Requirements and Their Significance
Every hospital policy is different, but most follow similar guidelines. Certain rules will depend on each facility’s circumstances, such as if it’s large to accommodate many visitors or if patient rooms are private.
Here are some of the most common practices and why they’re important.
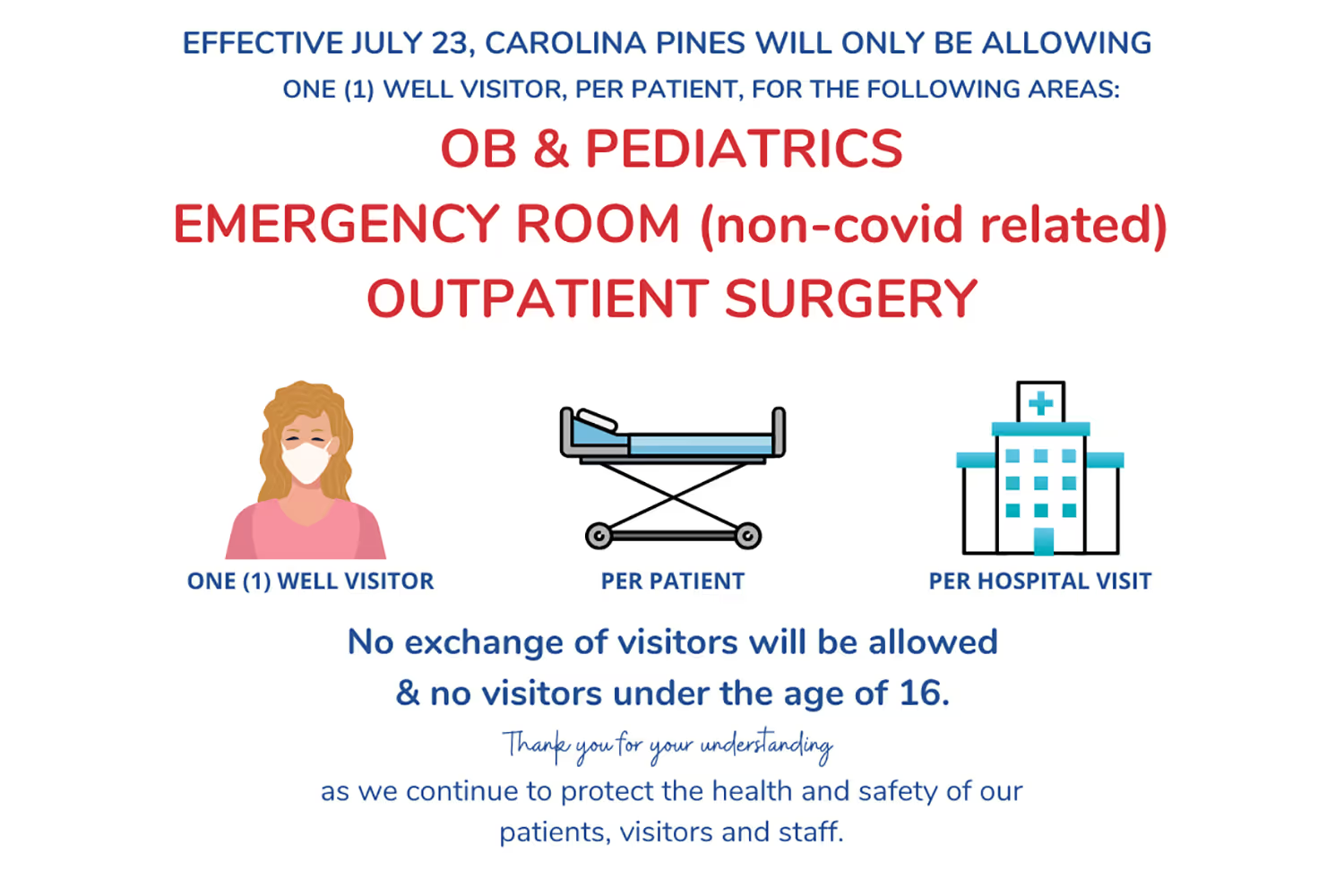
Limit Number of Visitors
Controlling the traffic in and out of hospitals contributes to patient health and safety. It reduces disruptions for those trying to heal, keeps people out of the staff’s way, and limits exposure to germs for everyone. Each hospital has a mass occupancy that’s safe, and this guideline keeps that under control.
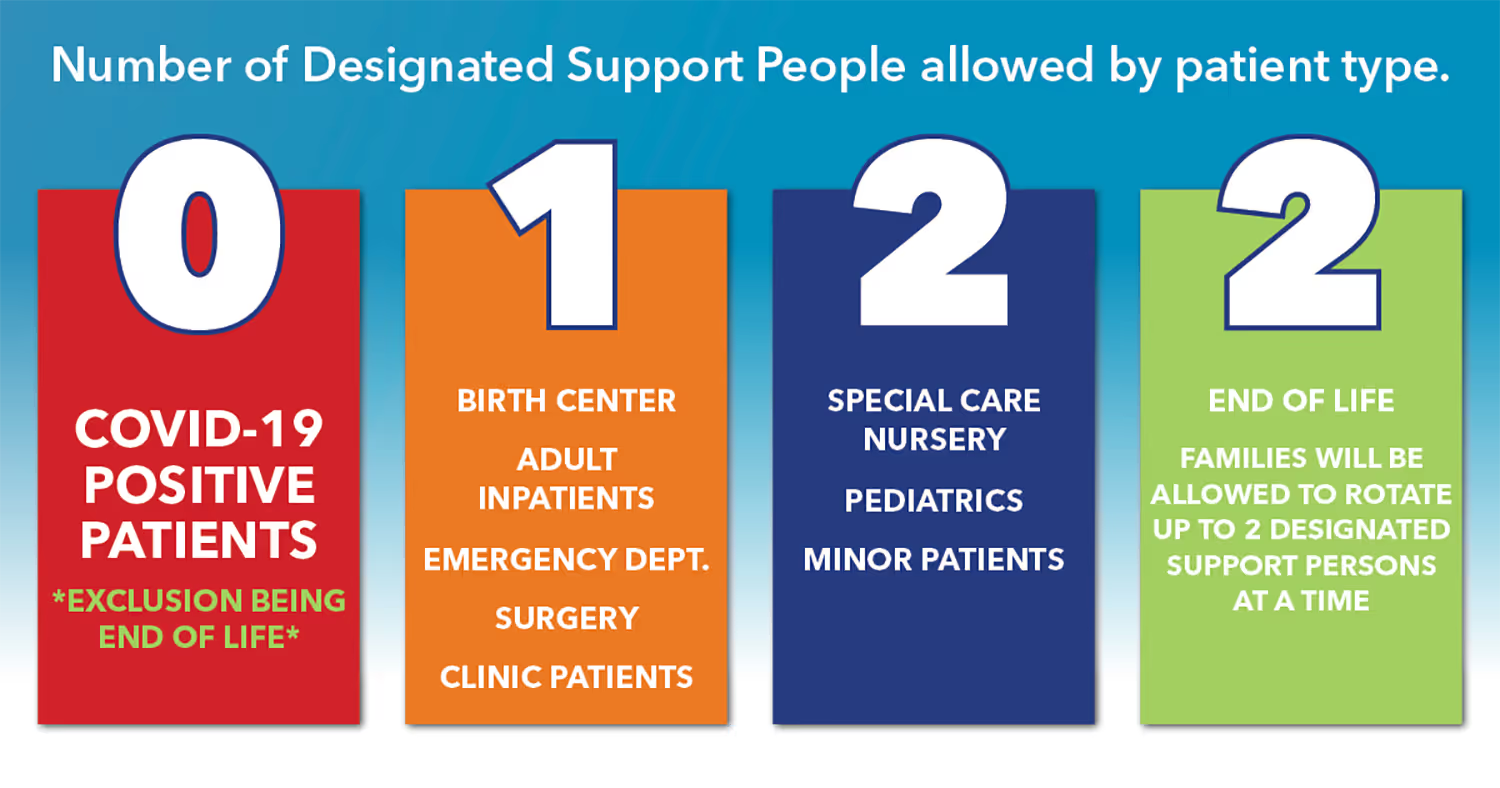
During the pandemic, these limits changed depending on the hospital. Many allowed only one visitor for adults or two adult caregivers for pediatrics per day.
Sign-In and Sign-Out
People should always check-in at the front desk so staff is aware of who is going in and out of rooms. It also helps them keep track of the number of visitors so that they follow the previous guideline. Signing out ensures that people aren’t staying longer than what’s reasonable for a patient’s recovery.
Giving them a visitor badge when they sign in is another security step. This helps staff keep track of who is there, who they came to see, and if they have permission to be there.

Get Permission From Patient
Some hospitals will confirm with the resident that they’re comfortable with having guests. They could feel too tired to enjoy the visit and just want to rest. Or they might not feel comfortable with certain individuals seeing them in the hospital and possibly hearing their PHI. Getting their permission is another step in protecting their confidentiality.
No Overnight Guests
Limiting public hours during the day helps control traffic so residents have the chance to rest. It guarantees some windows of time where there are fewer disruptions. It’s also safer since there is usually less staff at night, so they don’t need to keep track of other people coming in and out. In some situations, there may be exceptions such as if the patient can’t make their own health decisions.
Quiet Hours
Whether a hospital allows overnight guests or not, quiet hours are another way to aid in patients’ rest schedules. In the evening when things should be winding down, everyone needs to be mindful of making too much noise for those who are trying to sleep. And if the hospital does allow nighttime guests, these hours remind them that other people are trying to rest.
Cleanliness
Because hospitals have many germs and sick people, everyone coming in and leaving needs to take hygiene measures. To prevent guests from spreading germs, they should sanitize before entering rooms. It’s also necessary to do this before leaving and disinfect any belongings. This keeps them from taking germs home.

If a patient is in an isolation area, measures like personal protective equipment are necessary. Staff should help them correctly prepare with their PPE.
Some hospitals will also discourage gifts, food, balloons, and flowers. These can bring in germs and also common allergens like latex and pollen.
Do Policies Vary by Department?
The short answer to this question is yes, they can change depending on the hospital unit. Just like each facility may need its own rules, each department has its own needs as well.
A pediatric unit has different policies since most minors need parental consent for health decisions. Parents and guardians are essential caregivers to children. Limiting visitations can make children and parents feel isolated, stressed, overwhelmed, and anxious. Guardians have concerns with decision-making when they miss opportunities to engage in care.
Likewise, a labor and delivery department may deviate from the rest of the hospital’s policy. Even when people can’t stay overnight in other units, labor and delivery allow a support person for the mother.
Emergency and critical care units have different situations since they become chaotic at any moment. Extra people would get in the way of providing urgent care. Yet these patients are more vulnerable, so these departments may be flexible to allow a support person to stay. They may just restrict specific treatment areas to control traffic.
Psychiatric floors need to take extra precautions to protect their residents. People must go through a security check to confirm they aren’t bringing prohibited items. There are also special areas dedicated for visitations so staff can supervise. Most clinics also limit hours to prevent disruptions in therapy and mental health treatment.
Conclusion
Allowing visitors in hospitals can have positive impacts on patient recovery. It’s a way to make them more comfortable in an unusual, nerve-wracking environment.
But allowing unrestricted access to see patients isn’t safe, healthy, or practical. Because hospitals are stressful, residents need to get enough rest so they do recover. Having people come in and out all the time prevents this from happening.
It can also lead to other safety concerns such as more exposure to germs and more people in the way during emergencies.
When hospitals create these policies, it’s necessary to inform anyone that they exist so they know how to follow them and be mindful of others’ care. Telling them when they check-in and posting signs encourage them to comply. At first, it might seem like an inconvenience, but people will start to understand the significance.
Some facilities need different rules just like some departments may be more flexible or strict. Everyone has different needs so hospitals aim to accommodate them while protecting their clients so they can recover.
Emphasize your product's unique features or benefits to differentiate it from competitors
In nec dictum adipiscing pharetra enim etiam scelerisque dolor purus ipsum egestas cursus vulputate arcu egestas ut eu sed mollis consectetur mattis pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus mauris aliquam ornare nisl purus at ipsum nulla accumsan consectetur vestibulum suspendisse aliquam condimentum scelerisque lacinia pellentesque vestibulum condimentum turpis ligula pharetra dictum sapien facilisis sapien at sagittis et cursus congue.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Incorporate statistics or specific numbers to highlight the effectiveness or popularity of your offering
Convallis pellentesque ullamcorper sapien sed tristique fermentum proin amet quam tincidunt feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.

Use time-sensitive language to encourage immediate action, such as "Limited Time Offer
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Address customer pain points directly by showing how your product solves their problems
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Vel etiam vel amet aenean eget in habitasse nunc duis tellus sem turpis risus aliquam ac volutpat tellus eu faucibus ullamcorper.
Tailor titles to your ideal customer segment using phrases like "Designed for Busy Professionals
Sed pretium id nibh id sit felis vitae volutpat volutpat adipiscing at sodales neque lectus mi phasellus commodo at elit suspendisse ornare faucibus lectus purus viverra in nec aliquet commodo et sed sed nisi tempor mi pellentesque arcu viverra pretium duis enim vulputate dignissim etiam ultrices vitae neque urna proin nibh diam turpis augue lacus.


