Pro Tip for Providers: Effectively Applying the 8-Minute Rule
Each CPT code gets billed using either service-based units or time-based units. Those that use time-based units require more effort than just submitting how long the appointment was. Providers need to calculate the time it took for each task. They then identify how many units to include within the claim using the 8-minute rule.

If you’re new to working in healthcare, you may be feeling overwhelmed by the complexities of medical billing. Even if you’ve been here for a while, it’s still a challenge. There are so many different rules to properly code for the services you provided so that you can get paid.
You need to make sure that you do it right the first time so that you don’t end up with claim denials. After all, you won’t receive revenue until the insurance payer accepts the claim and reimburses you.
Yet these denials aren’t uncommon. One in seven claims gets denied, amounting to 200 million per day. 32% of hospital reimbursement leaders say that coding is their top concern for denials.
I’m not saying this to try to scare you. This is probably something you already knew. But of course, you don’t want to be a part of this statistic. To avoid common denials, you need to perfect your process of submitting bills to insurance.
But to make things more difficult, there are two different CPT coding methods for providers who have direct contact with patients, specifically physical therapists. Before we go any further, let me explain what a CPT code is. CPT stands for Current Procedural Terminology.
Healthcare professionals use these numerical codes to report the services they performed and provided to their patients. Essentially, these numbers tell the insurance payer what the physical therapist did and how much they should get reimbursed. Without proper coding, the provider will face the denials that I talked about before.
So now that you understand what these codes are, you’re probably wondering about those two different coding methods. Each CPT code gets billed using either service-based units or time-based units. Those that use time-based units require more effort than just submitting how long the appointment was.
Providers need to calculate the time it took for each task. They then identify how many units to include within the claim using the 8-minute rule. Yes, I do mean that there’s some math involved. Not all private insurance companies have adopted this rule, but every federal payer requires using it for billing.
By now, I might have confused you. But don’t fret. Service-based units are pretty simple. And once you get the hang of effectively applying the 8-minute rule, you’ll be able to correctly code using time-based units.
Service-Based vs. Time-Based Units
Before we get into the 8-minute rule, let me explain a little more about the difference between these units. I already said that service-based is easier to understand, so let’s start there. By its name alone, we know that service-based providers use these codes (duh).
Essentially, this rule applies to tasks that don’t denote time. For instance in physical therapy, this would apply to…
- An evaluation (97161, 97162, 97163, or 97164)
- Use of hot/cold packs (97010)
- Electrical stimulation (unattended) (97014)
Regardless of the amount of time it takes to complete these activities, the therapist can only bill for one unit per visit. This is why you might hear these referred to as visit-based units.
Like I said, pretty simple. This rule applies to specific codes. That means that the provider can’t just decide that they want to use this instead of time-based units. Each code gets designated as to which calculation method it requires. This makes it easier for the physical therapist to differentiate which type to use.
There are specific codes that get billed in increments of 15 minutes. As you might imagine, these codes are for the procedures that use time-based units. But how do providers account for this time if a treatment lasted less than 15 minutes, or the total time wasn’t an even 15-minute increment?
They use the 8-minute rule, of course. If you love math and numbers, you’re going to love using this. But if not, I’ll walk you through it so that by the end of this blog post, you’re a pro.
Simplifying the 8-Minute Rule
I already mentioned this, but it’s important to reiterate that the 8-minute rule does not apply to service-based codes. Those can only get billed once per visit, regardless of how long it took during the appointment. For example, a patient’s evaluation could take a majority of the visit length, but it still can only account for one unit.
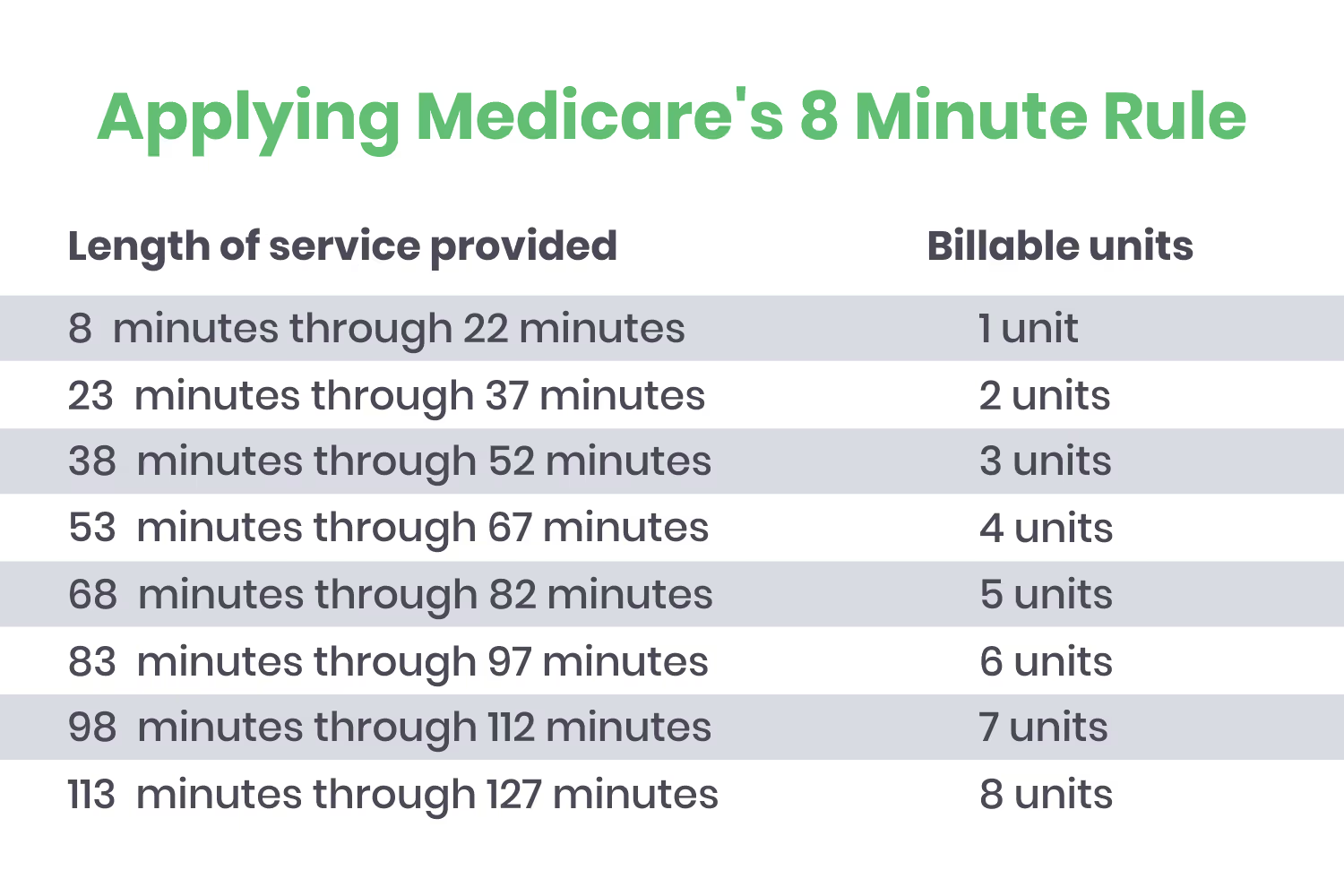
So let’s go over how to use the 8-minute rule for time-based codes. Providers can count a service as one unit if it lasted at least 8 minutes, but less than 22. This means that if a service was shorter than the 15-minute increment, the provider can still bill for it as long as it lasted at least 8 minutes. And if it was over 15 minutes, they can’t bill for a second unit until it lasts for more than 22 minutes (or, 8 minutes after the first 15-minute increment).
To help make sense of this, here’s a visual of the number of units you can bill for based on the time spent on a procedure or treatment.
Let’s go over a scenario for practice. Imagine that in one single visit, you offer 4 different services to a patient. The total appointment length is 75 minutes. You offer 23 minutes of therapeutic exercise, 17 minutes of manual therapy, 12 minutes of ultrasound, and 23 minutes of electrical stimulation unattended (ESUN).
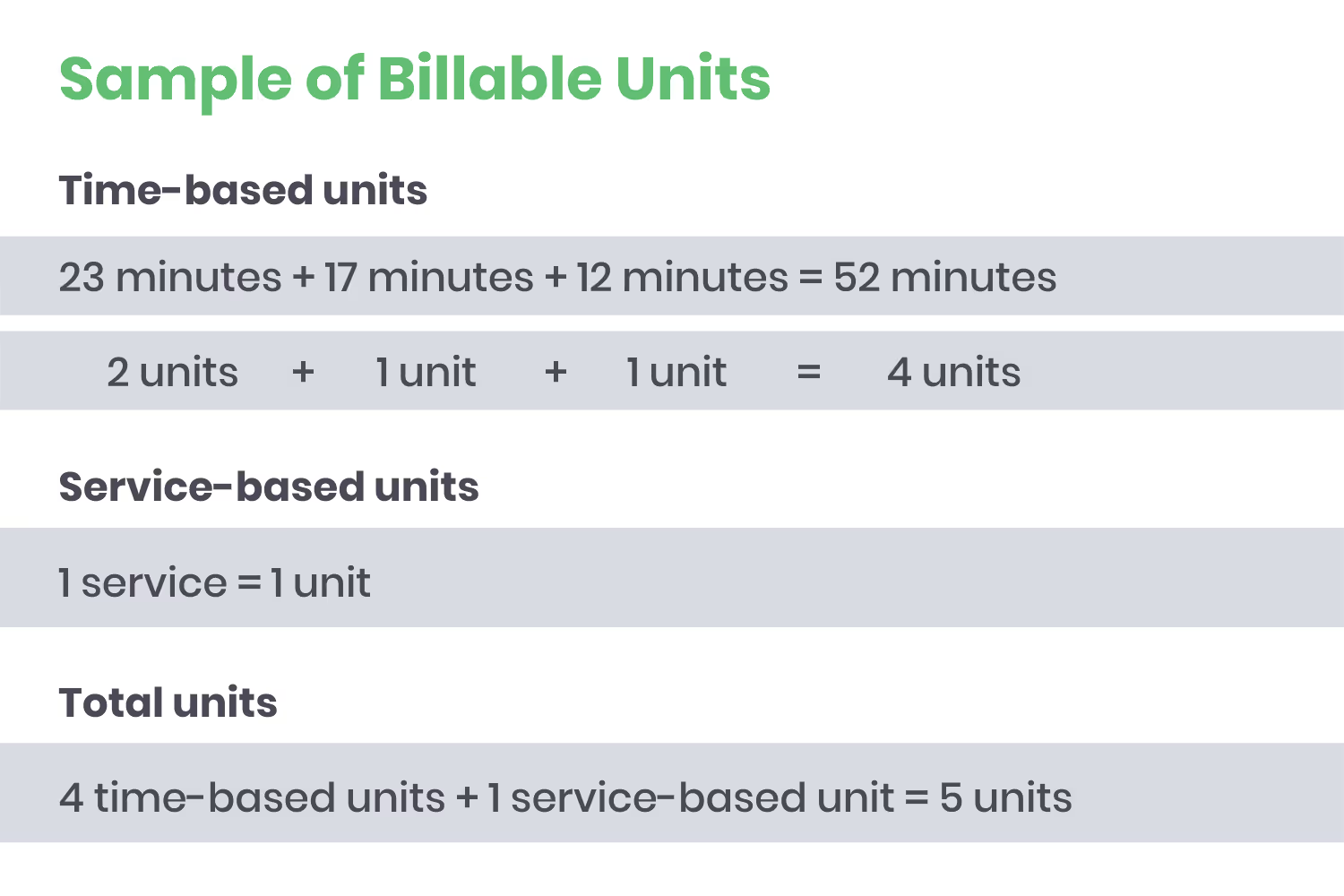
So how many units can you bill for? To calculate this using the 8-minute rule, you would add the time-based services: 23 + 17 + 12 = 52. This supports 4 billing units. The additional ESUN supports only one additional unit, despite the length of time it took since it’s a service-based unit and can only count for one. So in total, there would be 5 billable units.
If you’re a visual learner like myself, here’s the breakdown…
But what about mixed remainders? This is the combined remaining time between each of those services. Private insurers don’t usually allow for these. This means that you can only bill for the time of individual activities. But by Medicare and Medicaid guidelines, you can bill for mixed remainders. In this case, if the combined remaining time was 8 or more minutes, you could bill for an additional unit under the code for the procedure that took the longest time.
Services that Use the 8-Minute Rule
In the scenario above, I mentioned some specific time-based services which use the 8-minute rule. You might be wondering, “What are some other codes that use this?”
Here’s a list of some of the most common…
97032 Electrical Stimulation (manual)
97033 Iontophoresis
97034 Contrast Bath
97035 Ultrasound
97036 Hubbard Tank
97110 Therapeutic Exercise
97112 Neuromuscular Re-education
97113 Aquatic Therapy
97124 Massage Therapeutic
97140 Manual Therapy Techniques
97542 Wheelchair Management
97760 Orthotic Management
97761 Prosthetic Management
97762 Orthotic/Prosthetic Checkout
Avoidable Errors
Now that you know what this rule is, you can use it to avoid coding errors so you don’t end up with denials. To reiterate the issues that you need to prevent, here are some common avoidable errors when applying this rule.
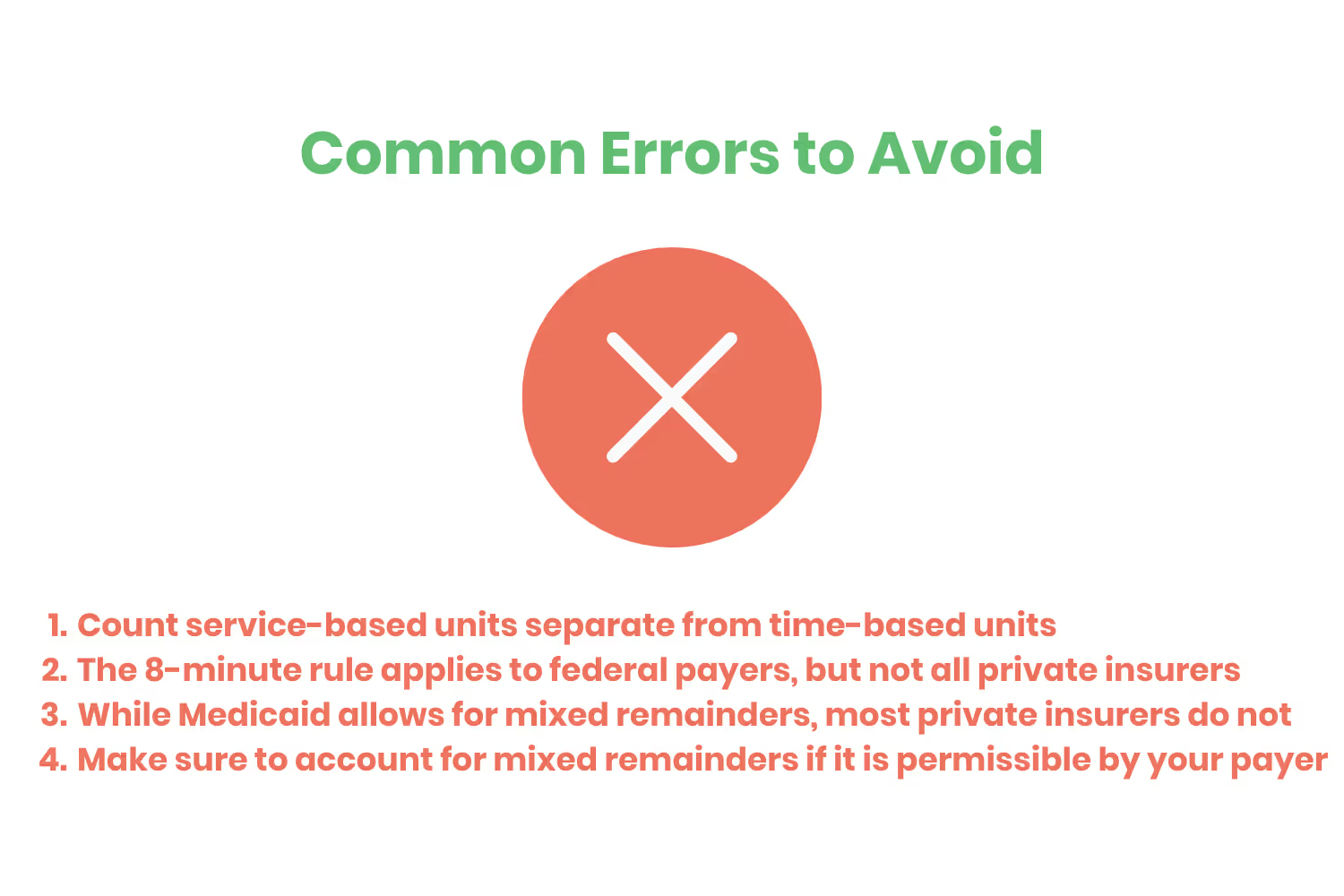
- Count the service-based units separate from time-based units. They only count as one billable unit, regardless of their length of time, so their time should not get added with the time-based procedures.
- The 8-minute rule applies to federal payers, but not all private insurers. If your payer doesn’t follow Medicaid’s guidelines, you need to confirm that you are billing in agreement with their terms.
- Most private insurers don’t allow for mixed remainders. If this is the case, you must bill each unit based on the individual activities.
- If accounting for mixed remainders is permissible by your payer, make sure to include that additional unit.
Conclusion
As a healthcare provider, there’s a lot on your plate. You already need to offer treatment to so many patients. This makes it more of a challenge to manage administrative tasks, such as medical billing.
But this isn’t something you can let fall to the wayside. Without proper coding, claims will just end up denied and you won’t receive reimbursement. This is stating the obvious, but that’s not something you want.
Health professionals that have direct contact with patients provide two different types of procedures: service-based and time-based. As if coding wasn’t already complicated enough, each of these follows different billing rules.
Hopefully, by now you have a better understanding of how to effectively apply the 8-minute rule for time-based units. Calculating these total units ensures that you…
- Don’t leave out any billable time
- Don’t bill for too many units
Knowing how to identify these versus service-based units also makes it possible to calculate the correct total number of billable units. You won’t accidentally apply the 8-minute rule to the service-based units, because you’ll know how to count them separately.
By following all of these steps and avoiding common billing mistakes, you’re on your way to properly submit claims to payers so you can receive revenue quickly.
Emphasize your product's unique features or benefits to differentiate it from competitors
In nec dictum adipiscing pharetra enim etiam scelerisque dolor purus ipsum egestas cursus vulputate arcu egestas ut eu sed mollis consectetur mattis pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus mauris aliquam ornare nisl purus at ipsum nulla accumsan consectetur vestibulum suspendisse aliquam condimentum scelerisque lacinia pellentesque vestibulum condimentum turpis ligula pharetra dictum sapien facilisis sapien at sagittis et cursus congue.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Incorporate statistics or specific numbers to highlight the effectiveness or popularity of your offering
Convallis pellentesque ullamcorper sapien sed tristique fermentum proin amet quam tincidunt feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.

Use time-sensitive language to encourage immediate action, such as "Limited Time Offer
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Address customer pain points directly by showing how your product solves their problems
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Vel etiam vel amet aenean eget in habitasse nunc duis tellus sem turpis risus aliquam ac volutpat tellus eu faucibus ullamcorper.
Tailor titles to your ideal customer segment using phrases like "Designed for Busy Professionals
Sed pretium id nibh id sit felis vitae volutpat volutpat adipiscing at sodales neque lectus mi phasellus commodo at elit suspendisse ornare faucibus lectus purus viverra in nec aliquet commodo et sed sed nisi tempor mi pellentesque arcu viverra pretium duis enim vulputate dignissim etiam ultrices vitae neque urna proin nibh diam turpis augue lacus.




