Denial Code CO 252: Everything You Need to Know
One of the most common denial codes is CO 252. That’s exactly the code that we’re going to take a deep dive into in this blog post.

One-third of all submitted claims get denied or ignored on the initial submission.
That doesn’t sound great, but if you flipped the script you’re still receiving 66% of your claim revenue. That’s still pretty good, right?
Well, let’s look at it on a large scale. In 2021 hospitals lost an average of $5 million to their total revenue due to denied claims.
Even if you don’t work at a hospital, those losses trickle down to similar numbers for smaller healthcare organizations.
The point I’m trying to make is that denials lead to massive financial bottlenecks that could result in serious losses. In some cases, those losses have been so significant that healthcare organizations have had no choice but to close their doors for good.

But, if they’re an issue across the entire healthcare industry that even giant hospital systems struggle with…what can you do?
In order to answer that question, we need to break down a few more statistics.
The truth is that 60% of denied claims are never resubmitted. Choosing not to resubmit claims that have a denied status is literally leaving money on the table. There’s no way of sugar-coating.
Of course, resubmitting a denied claim requires a bit of work. You need to fix the error cited by the insurance company (more on that later) and resubmit it. That takes effort and time…which costs money.
At some point, the efforts associated with correcting and resubmitting a claim have to outweigh the cost of writing it off as a loss, right?
Well, the average cost to rework and resubmit a claim averages to ~$25 per claim for practices and ~$181 per claim for hospitals.
Although those dollar amounts might seem as though they’re painting a dismal picture, we can’t take them at face value.
There’s a pattern to claim denials. In fact, it’s very likely that you have multiple returned claims with the same denial code. In other words, having a sound denial management process means understanding those patterns and educating yourself and your staff on fixing them. Achieving those two steps guarantees that your per claim correction costs decrease well below the averages I just gave you.
Since we’ve been in business as a medical claims clearinghouse since 1999, we’ve noticed that certain denial types appear more often than others.
One of those denial codes is CO 252. That’s exactly the code that we’re going to take a deep dive into in this blog post.
What is denial code CO 252?
From a technical standpoint, denial codes are also known as claim adjustment reason codes (CARC).
CO 252 starts with “CO”. This “CO” portion stands for “Contractual Obligation”.
What the heck does that last sentence mean?
Well, a denial that includes “CO” is one that signifies a denial based on the contract and as per the fee schedule amount. CO is one of the biggest and most common categories of denials. It has more than 200 distinct code combinations.
Insurance companies often place denials into the CO category when one of two things happen. Either, there is a joint payer/payee regulatory obligation that leads to an adjustment not attributable to the member. Or the provider’s fees surpass the reasonable and customary amount for which the patient is accountable.
In either case, providers are solely financially responsible when they receive a CO denial. In other words, patients and/or beneficiaries don’t receive any financial responsibility for these denials.
CO 252 means that the claim needs additional documentation to support the claim.
Although this denial reason code seems straightforward and easy to understand. In practice, this code can get dicey very quickly.
You see, it’s really vague. The code literally means that the claim you submitted is missing information. It doesn’t tell you what you’re missing.
Thus, this denial code should come with a remittance advice remark code (RARC) attached to it. It can’t exist by itself.
Common CO 252 RARCs
In a perfect world, RARCs come attached alongside CARCs as they provide more specific information as to what happened to the denied claim.
CO 252 is such a general denial code that you simply cannot figure it out without some added color. It’s simply too generic of a code to exist on its own.
If you thought the 200 different combinations of CO denial codes were a lot, wait until you read this number. X12 lists over 1,200 different RARC codes on its website. Yikes.
Luckily, the Council for Affordable Quality Healthcare (CAQH) published its “CORE” rules. CAQH published this set of rules to help standardize CARC and RARC combinations for both insurance and healthcare organizations.
Now that they’re published, we can all live happily ever after in the revenue cycle world and never have any issues. I’m being facetious.
The truth is that even though they exist, it doesn’t mean that the payer has a requirement to send back this denial code with its recommended RARC attached to it. Although rare, this is a very frustrating experience when it happens.
You can download and view the “CORE” rules yourself as CAQH makes them readily available on its website. It’s definitely helpful, but even if you do download it…there are 111 different RARC combinations associated with denial code CO 252.
This is where our multiple decades of experience as a clearinghouse helps. Let’s take a look at some of the most common RARCs that we see attached alongside CO 252.
- N479: Missing Explanation of Benefits (Coordination of Benefits or Medicare Secondary Payer).
- N710: Missing notes.
- N712: Missing summary.
- N714: Missing report.
- N716: Missing chart.
Can I ignore denial code CO 252?
Ignoring your denials, no matter what code they are is never a good idea. Yes, there are some codes out there that aren’t fixable due to where the mistake happened along the claim’s journey.
I’ll walk you through a workflow that you could implement and reap the benefits of today in the next section, but first, let’s understand the importance of not ignoring this code.
By now you know that correcting this type of denial code isn’t always a smooth process. It’s a real bummer when you receive this code and the insurance organization didn’t attach a RARC to it because of its generalized definition.
But, the risk of you running into that scenario shouldn’t cause you to ignore it due to how common this denial code is. There is serious revenue on the table here.
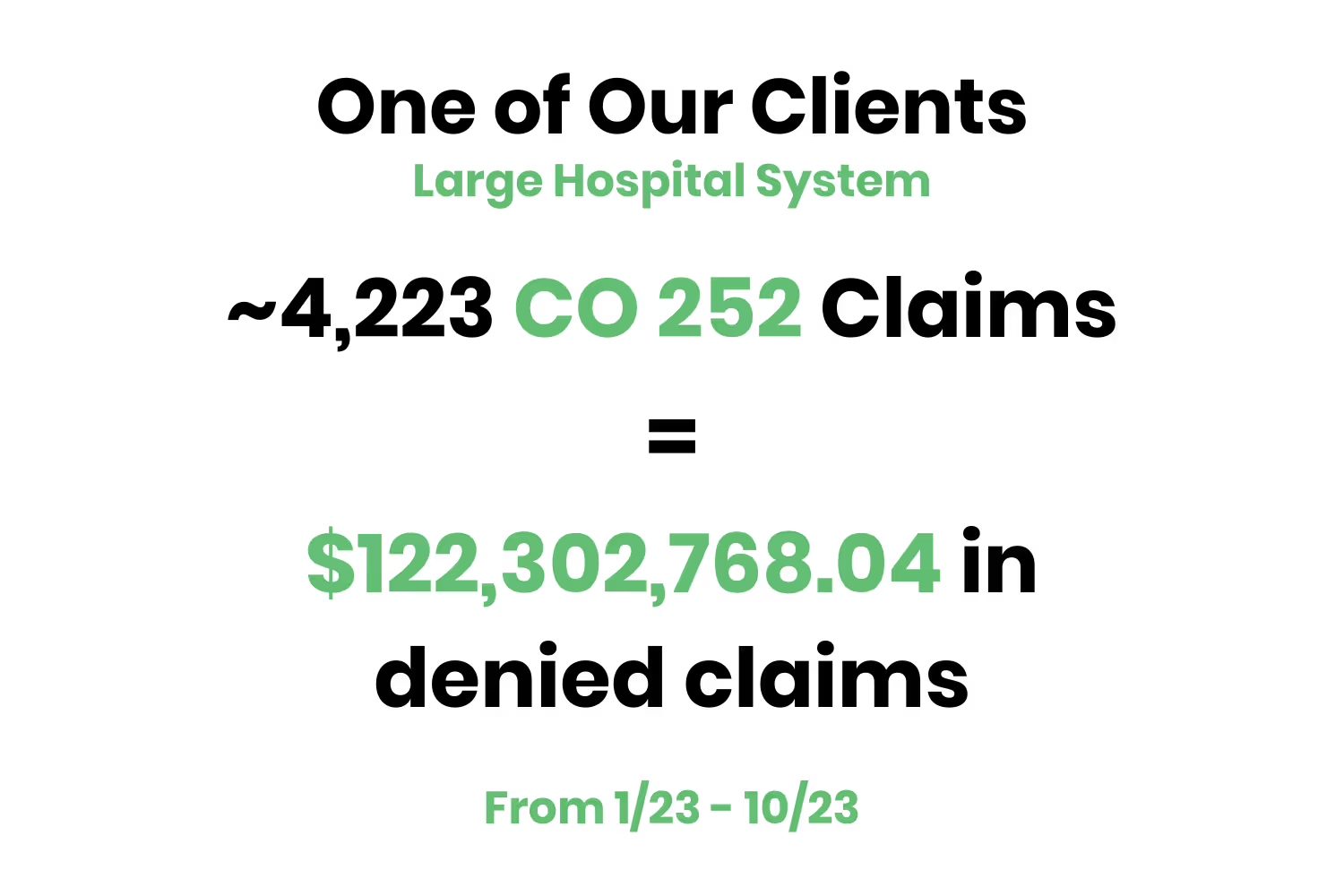
Let’s look at an example of a large hospital system that we’re currently working with to help fix their denial environment.
This system had 4,223 CO 252 denials from January 1, 2023, to the time of this blog. From a dollars perspective that’s equal to $122,302,768.04 in revenue!
Of course, this example is on a larger scale given it’s a hospital system. However, the losses are still there for smaller healthcare organizations as well since this code is so common.
So, should you ignore CO 252? No.
What's the best way to manage denial code CO 252?
As I alluded to in the introduction to this blog post, the majority of denials are overturnable…you just need to know what to look for.
Based on the previous section, you now possess the knowledge on how to quickly identify the specific issue associated with a CO 252 denial. You also now know that sometimes insurance organizations don’t include RARCs that provide further reasoning associated with this type of denial.
With those two aspects in mind, you can now quickly look through all of your CO 252 denials and prioritize them quickly.
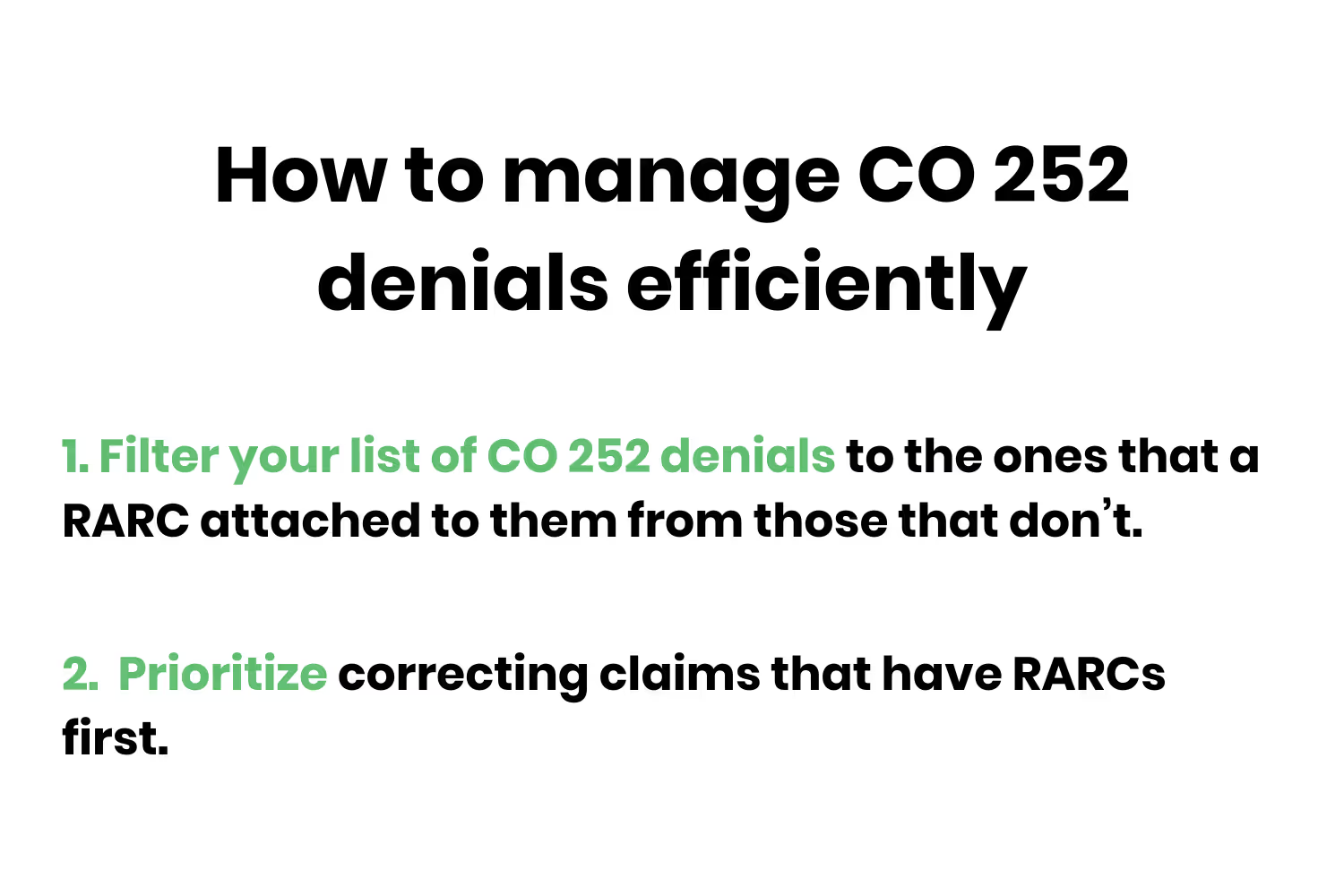
This process is simple. Look at the list of your CO 252 denials and filter the ones that a RARC attached to them from those that don’t. Correct those that have a RARC and resubmit them.
Things do start to get a little tricky for the denials with that code that don’t have a RARC. You’ll have to contact that payer either by calling them or contacting them through their portal. Working through these denials is still worth it, but the cost associated with correction for them increases quite a bit.
If the name of the game for you is to increase your collections associated with your denials…this workflow with CO 252 denials will help tremendously. If you need help with the ones that don’t have a RARC associated with them, your best bet is to partner with an experienced clearinghouse (like us).
Either way, ignoring this denial code is NOT a great idea.
Conclusion
It’s ironic that just a few sections ago within this blog post I mentioned that denial code CO 252 had a simple definition. Several sentences and hundreds of words later and we’ve come a long way.
Although I still stand by the fact that its definition is easy to comprehend, there are aspects to it that require some maneuvering. This goes back to the point all the way from the introduction to this post. A healthy denial management environment isn’t about muscling through it and hoping for returns.
It’s about recognizing patterns and prioritizing your correction workflow on the same. And achieving that can’t happen without educating you and your team on specific, common denial codes.
Emphasize your product's unique features or benefits to differentiate it from competitors
In nec dictum adipiscing pharetra enim etiam scelerisque dolor purus ipsum egestas cursus vulputate arcu egestas ut eu sed mollis consectetur mattis pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus mauris aliquam ornare nisl purus at ipsum nulla accumsan consectetur vestibulum suspendisse aliquam condimentum scelerisque lacinia pellentesque vestibulum condimentum turpis ligula pharetra dictum sapien facilisis sapien at sagittis et cursus congue.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Incorporate statistics or specific numbers to highlight the effectiveness or popularity of your offering
Convallis pellentesque ullamcorper sapien sed tristique fermentum proin amet quam tincidunt feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.

Use time-sensitive language to encourage immediate action, such as "Limited Time Offer
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Address customer pain points directly by showing how your product solves their problems
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Vel etiam vel amet aenean eget in habitasse nunc duis tellus sem turpis risus aliquam ac volutpat tellus eu faucibus ullamcorper.
Tailor titles to your ideal customer segment using phrases like "Designed for Busy Professionals
Sed pretium id nibh id sit felis vitae volutpat volutpat adipiscing at sodales neque lectus mi phasellus commodo at elit suspendisse ornare faucibus lectus purus viverra in nec aliquet commodo et sed sed nisi tempor mi pellentesque arcu viverra pretium duis enim vulputate dignissim etiam ultrices vitae neque urna proin nibh diam turpis augue lacus.




