How to Speed Up Your Denied Claims Resubmission Process
It’s inevitable as a healthcare organization you will face denied claims. When you do receive them, what’s the next step? We’ve broken down different facets of the resubmission process to help you visualize how you can get paid quicker.
Everyone knows the famous quote from Benjamin Franklin, “Nothing is certain except for death and taxes.”
If he was still alive and also happened to be a doctor, he’d change his saying to, “Nothing is certain except denied claims.”

No matter how perfect you think your medical practice is, at some point, you’ll receive denials.
They are such a common occurrence that Change Healthcare estimated that $262 billion worth of claims submitted in 2017 were initially denied.
Why are they so common? The claim submission process is too intricate. There are thousands of variables at play when submitting a claim.
So it’s not a matter of if you’ll receive denied claims, it’s a matter of when.
When you do receive them, what’s the next step? How can you diagnose, correct and resubmit them within a reasonable amount of time without spending an excessive amount of money?
Research the proper claim deadlines
As we know, every insurance company has a provider manual.
From a medical billing perspective (and for the scope of this blog post) these manuals may contain four important deadlines; timely filing, claim resubmission, claim reconsideration and appealing.
Each deadline defines an acceptable amount of time for submission during different situations. If you do not abide by these deadlines, you will have a denied claim on your hands that won’t help you receive payment.
- Timely filing defines the deadline to submit a claim after service is rendered on a patient.
- Claim resubmission is a deadline for claims that were denied for missing documentation, incorrect coding, etc. which now has the required information.
- Claim reconsideration happens when there is a request to review a claim that a healthcare provider feels it was either incorrectly paid or denied due to errors during processing.
- An appeal is a request to change a reconsideration decision, an initial review decision, or an initial claim decision.
Arizona Healthcare Cost Contain System
As an example, let’s take a look at a payer who has definitions for three of the four deadlines above, Arizona Health Care Cost Containment System (AHCCCS).
Although specific, they are a great example. They give clear definitions and deadlines for what they consider to be a resubmission and reconsideration while explaining their special requirements.
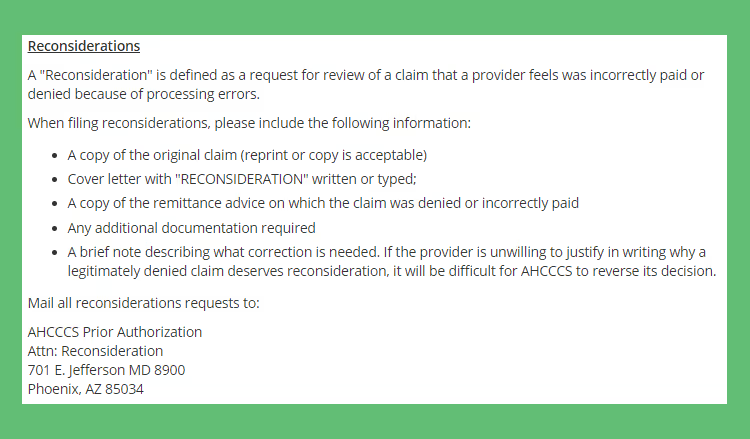
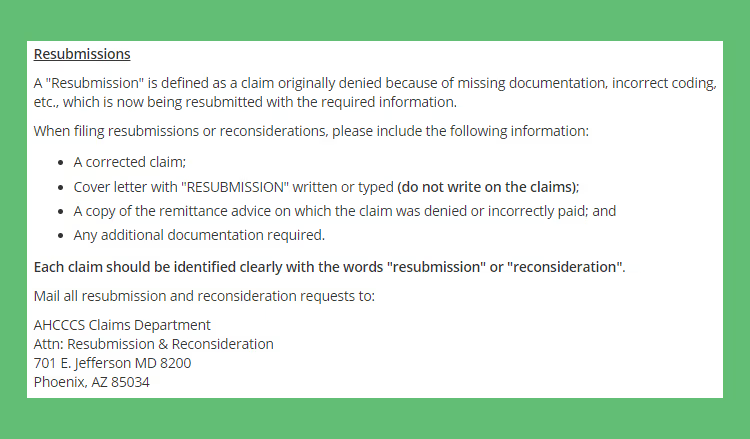
Whether you are sending a resubmission request or a reconsideration request, AHCCCS’ deadline is 12 months from the date of service.
Aetna
As another example, let’s look at a larger healthcare payer. This time let’s look at Aetna. Aetna gives definitions for reconsiderations and appeals. They also include what they need to resolve a dispute.

Aetna’s claim reconsideration deadline is 180 calendar days from the initial claim decision while their appeal deadline for resubmitting denied claims is 60 calendar days of the previous decision.
We looked at only two insurance payers and found four different deadline definitions, three different deadlines and three different lists of requirements to resubmit your denied claims.
Multiply the different deadlines and requirements above by the variety of different payers your patients use.
In practice, you see hundreds of patients a week. The chances that all of them have only a handful of different healthcare insurances is slim.
Understanding your payer mix and putting their deadlines all in one place will make it easier for you to resubmit your denied claims.
Realize your most common denied claims
This may seem like an outlandish statement but the best part about receiving denied claims is that each of them gives you a reason why they weren’t accepted.
Once you have an overview of what types of denials you experience most often, you can analyze each one and theorize if an internal process is a direct cause.
Let’s breakdown 20 of our client’s most common types of denied claims…
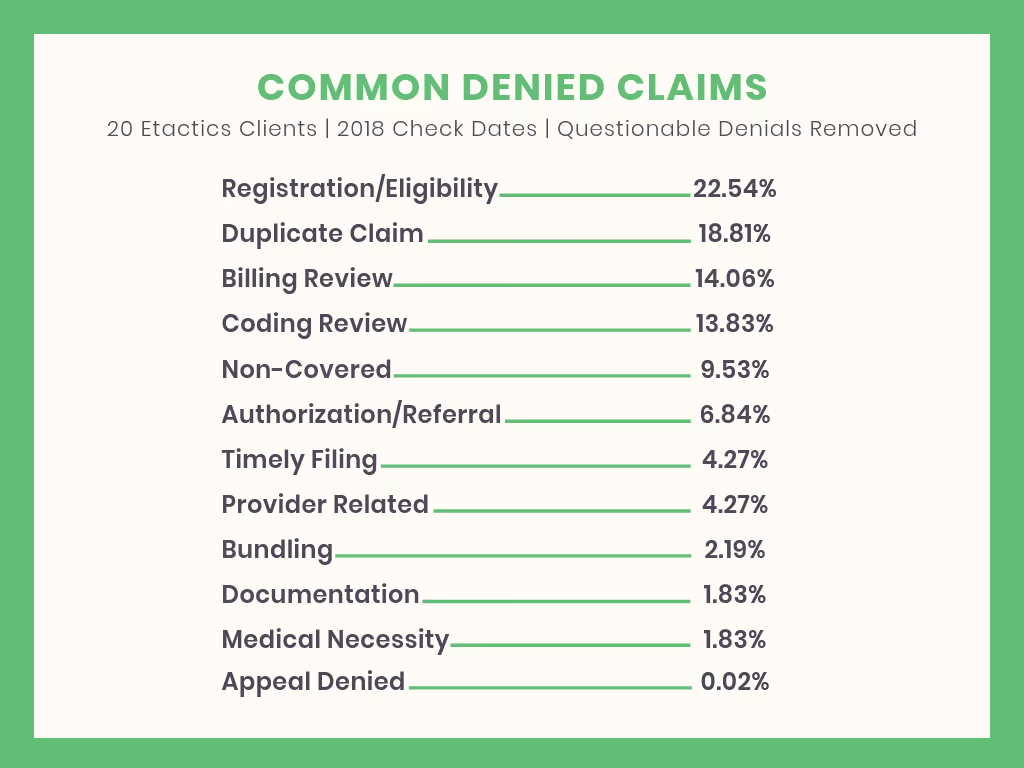
When creating the graph above we grouped together a handful of different Claim Adjustment Reason Codes (CARC) and Remittance Advice Remark Codes (RARC) for a better representation.
The two most common types of denied claims from 20 of our clients relate to Registration/Eligibility at 22.54% and Duplicate Claims at 18.81%.
Now let’s analyze what these could mean and how they can be fixed...
- Maybe they are using the outdated process of not checking their patient’s eligibility on a consistent basis. If so, they could implement a process where their staff checks their patient’s eligibility before they come in to visit.
- It’s possible that they don’t have a solution that checks their patient’s eligibility. If that’s true and they are checking everything manually, they’re wasting a lot of time and should evaluate automated eligibility solutions.
- Maybe they do have an eligibility solution but their staff doesn’t know how to properly use it. If that’s the case then they need to educate and train their staff on the in’s and out’s of the solution.
The point is, every healthcare provider will have a different mix of denials and that’s not a bad thing. Your denied claims help notify you of outdated or ineffective processes. Once identified and corrected, you’ll see an increase in your revenue immediately.
Conclusion
On top of seeing hundreds of patients every week you need to submit claims, prep denials for resubmission, and submit them to your payers. Each of those steps has a mandated deadline placed upon it that is out of your control. So what’s the best way to speed up your resubmission process for denied claims?
After you’ve documented all of the different definitions and deadlines associated with your payer mix take a look at your data. What’s the shortest reasonable deadline?
Use the shortest reasonable deadline as your goal time for everything you do involving claims. It doesn’t matter if it’s for timely filing, reconsideration, resubmission, or appeal requests. Using the shortest time will always ensure…
- Everything you submit or resend will fall within all deadlines.
- Your staff will have a clear and concise number of days they have when working with your claims.
- All of your denials related to these deadlines will immediately decline.
Emphasize your product's unique features or benefits to differentiate it from competitors
In nec dictum adipiscing pharetra enim etiam scelerisque dolor purus ipsum egestas cursus vulputate arcu egestas ut eu sed mollis consectetur mattis pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus mauris aliquam ornare nisl purus at ipsum nulla accumsan consectetur vestibulum suspendisse aliquam condimentum scelerisque lacinia pellentesque vestibulum condimentum turpis ligula pharetra dictum sapien facilisis sapien at sagittis et cursus congue.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Incorporate statistics or specific numbers to highlight the effectiveness or popularity of your offering
Convallis pellentesque ullamcorper sapien sed tristique fermentum proin amet quam tincidunt feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.

Use time-sensitive language to encourage immediate action, such as "Limited Time Offer
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Address customer pain points directly by showing how your product solves their problems
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Vel etiam vel amet aenean eget in habitasse nunc duis tellus sem turpis risus aliquam ac volutpat tellus eu faucibus ullamcorper.
Tailor titles to your ideal customer segment using phrases like "Designed for Busy Professionals
Sed pretium id nibh id sit felis vitae volutpat volutpat adipiscing at sodales neque lectus mi phasellus commodo at elit suspendisse ornare faucibus lectus purus viverra in nec aliquet commodo et sed sed nisi tempor mi pellentesque arcu viverra pretium duis enim vulputate dignissim etiam ultrices vitae neque urna proin nibh diam turpis augue lacus.




