65+ Modern Medical Billing Denials Statistics
To truly combat the issue and improve your bottom line, you need to understand the denial landscape. The 65+ medical billing denial statistics below can give you insight into the root cause of denied claims.

The medical billing denial management market size in the U.S. is enormous. In 2021, it had a value of $3.57 billion. Experts predict that by 2027, it will reach $5.94 billion.
Why would this niche healthcare marketing be worth so much?
Well, insurance claim denials are a big problem in the healthcare industry. A denied claim leads to lost revenue for healthcare entities, causing major financial losses. If a practice suffers from too many denied claims, it could go bankrupt and close!
So what is a claim denial?
A claim denial happens when an insurance provider rejects a request to pay a medical bill. The payor first receives the request and depending on the information, will decide to pay in full, partially pay, or deny the claim.
How often does this happen?
In 2021, there were 48.3 million denied claims, accounting for 16.6% of all in-network claims submitted that year. But this doesn't mean that the denied claims are evenly distributed across the board. When it comes to in-network claims, insurer denial rates ranged from 1% to 80%.

If you’re a healthcare provider, you likely deal with denied claims regularly. Of course, receiving them doesn’t mean you should lose all hope. In most cases you can appeal them, but that still requires a lot of effort.
To truly combat the issue and improve your bottom line, you need to understand the denial landscape. The 65+ medical billing denial statistics below can give you insight into the root cause of denied claims.
Denials are Rising
Health insurance claim denials are rising.
According to Change Healthcare, from 2016 to the beginning of 2020, the average denials rate increased by 20%. By the end of 2020, the total increase sat around 23%. Part of this is because the rate naturally increases over time. But even so, the percentage of denied claims increased exponentially due to the 2020 COVID-19 pandemic.
To illustrate this, in 2016 the average rate of denied claims sat around 9% of all claims submitted. By June 2020, while at the crisis point of the COVID-19 pandemic, the average rate was 10.8%. By quarter 3 of 2020, the average rate hit 11.1%.
To make matters worse, 30% of people who responded to Experian Health’s survey say denials are increasing between 10%-15%.
Why are they rising?
The three primary reasons according to Experian are…
- Data analytics (62% of people say this)
- Lack of automation in the claims and/or denials process (61% of people say this)
- Lack of thorough training (46% of people say this)
In truth, healthcare providers lack experienced resources to help prevent denials. This is especially true in complex clinical cases. They lack the expertise to support appeals and data for root cause analysis.
Staff attrition and training are also a problem. With a tight labor market, hiring and retaining qualified staff members becomes harder and harder. The complexity of denials requires robust training and education programs.

Unfortunately, companies oftentimes don’t have the time or the resources to follow through. It’s a requirement for clinical staff to manage clinical denials, but when overwhelmed by patient care, claim management falls by the wayside.
It also doesn’t help that there’s a growing backlog of denials. Peak seasons and staffing challenges expand lead to such workflow bottlenecks.
With timely filing deadlines, many of these aren’t filed in time and end up in the denied pile. Many healthcare practices focus on remedying individual denials instead of analyzing the root causes. Not only does this continue the cycle of producing denials, but it also fails to reduce the volume of current denials.
Denials by Region
Needless to say, the pandemic screwed everything up when it came to healthcare entities trying to work with insurance companies for payment of services provided.
Interestingly enough, the areas most affected by the first wave of outbreaks were the same areas with the highest denial rates.
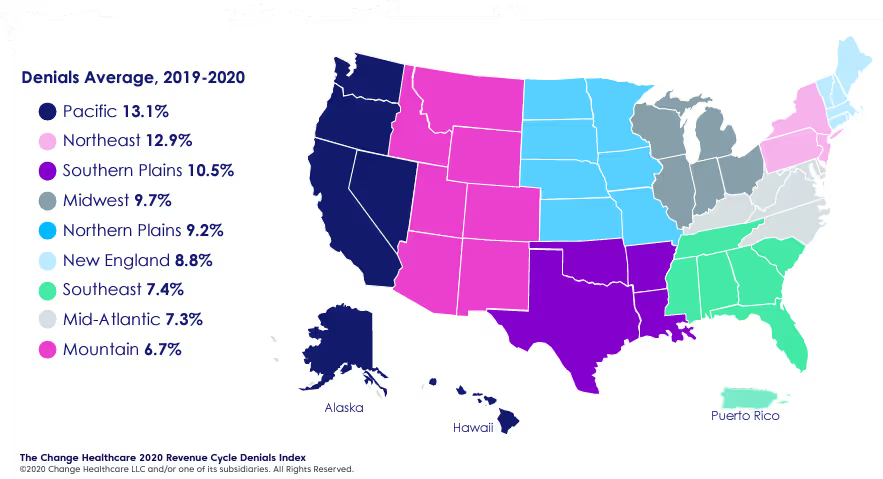
As you can see from the picture above, the Pacific area had the worst denial average of 13.1%. More specifically, during the first quarter of 2020, the Pacific area had a whopping 13.85% claim denial rate. Although this may not seem like a big difference at first glance, it's still 11.7% more than the denial average 12 months prior.
Next in line is the Northeast housing in New York City with an average denial rate of 12.9%. During Q1 of the pandemic, the Northeast area had a denial average of 13.63%. This means that in 12 months, their denial rate increased by 12.2%.
After the pandemic, a few things changed. The top five average denial rates for in–network claims by Healthcare.gov issuers in 2021 are…
- Indiana at 29%
- Mississippi at 29%
- Georgia at 26%
- Texas at 24%
- Arkansas at 24%
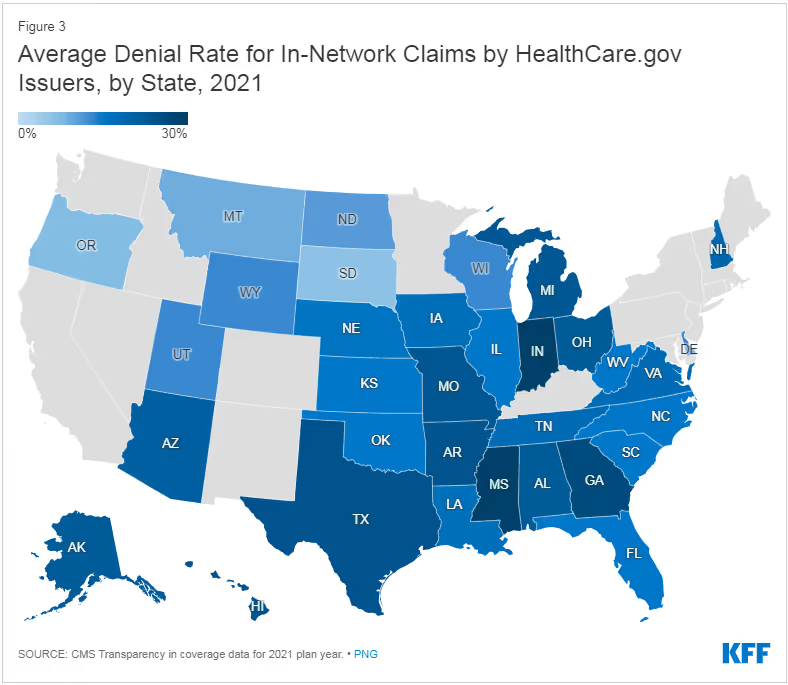
It’s important to take this information with a grain of salt. After all, HealthCare.gov doesn’t operate in most of the western coastal area or the northeast.
Since these two areas were most heavily affected by denied claims during the height of the pandemic, the information illustrated in the picture above may be misleading.
Keep this in mind as you evaluate the condition of your state.
Denials Affect ROI
As I mentioned before, denials lead to revenue losses.
But, how often are claims denied and how significant is the impact on your bottom line?
73% of healthcare organizations say that they see denied claims 5%-15% of the time. More specifically, nearly one in three organizations see denied claims 10%-15% of the time.

This means that a third of healthcare entities lose about a tenth of their revenue on any given day. In other words, that’s billions of dollars that may or may not ever see reimbursement.
Talk about placing unnecessary pressure on the provider's cash flow and revenue cycle.
The overhead to rework and submit these claims can be significant and further dilute reimbursement totals.
That said, the majority of organizations are trying to do something about the situation. 52% of survey respondents upgraded or replaced their claim processing technology in the last 12 months. Despite this, more than 75% companies are at least somewhat likely to replace their existing claim management solution if the new solution could improve their ROI.

What does better ROI mean to these companies?
Depending on who you ask, you’ll get different answers.
- 61% say that one of the metrics they use to determine ROI is the hours spent appealing or submitting claims.
- 52% say that it is the time spent appealing and resubmitting claims versus the reimbursement totals.
- 47% say that it is the rate of clean claims.
- 41% say it is the denial rate.
Becoming a Priority
Dealing with denials means dealing with withhold revenue. Because of their negative impact, nearly 3 out of 4 providers indicate that reducing denials is a high priority.
For 70% of Experian survey respondents, claims management is more important now than it was before the pandemic.

This change happens because of four main reasons…
- 67% say it’s because payer policy changes are happening more frequently.
- 51% say it’s because reimbursements are taking longer.
- 43% say it’s because errors on claim submissions are increasing.
- 42% say it's because the volume of denials is increasing.
This means that the reason many healthcare entities care about denied claims is that they are becoming more of a problem.
Of the 42% of organizations that said denials are increasing, they list the following as operational challenges causing the denials…
- 62% say it’s due to insufficient data and analytics to identify submission issues.
- 61% say it’s due to a lack of automation in claim submissions and/or denial prevention processes.
- 46% say it’s because of a lack of training.
- 44% say it's because of a lack of in-house expertise.
- 33% say it's due to dated technology that is inadequate for the work that needs to happen.
- 30% say it’s due to staffing shortages.
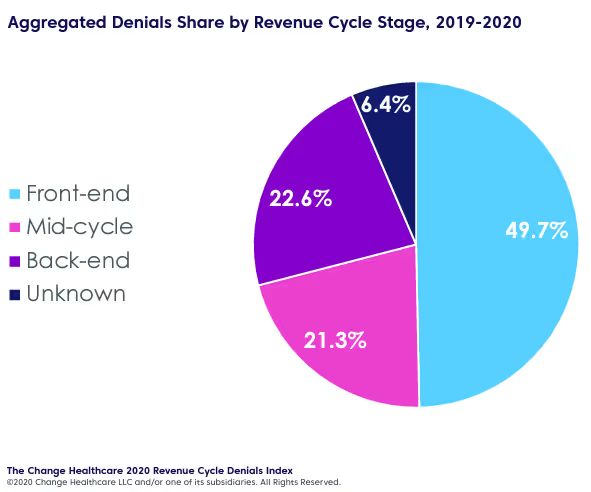
The Origins of Denials
The leading cause of denials occurs in the front-end cycle of denials. In fact, registration and eligibility are the leading cause of health insurance claim denials. This involves the coordination of benefits, benefit maximum, plan coverage, and more.
According to Change Healthcare, the top 5 causes of denials are…
- Registration/eligibility (26.6%)
- Missing or invalid claim data (17.2%)
- Authorization/pre-certification (11.6%)
- Service not covered (10.6%)
- Medical Documentation requested (9.2%)
Three of these five main causes happen at the front end of the revenue cycle. This means that the problems arise while the patient is still in the building. To illustrate this further, roughly half of all denials happen in the front end of the revenue cycle.
On the other hand, Experian asked survey respondents to list the top three reasons they see denials. The percentages indicate how often someone ranked the associated reason first when selected.
- 48% - Authorizations
- 42% - Provider eligibility
- 42% - Code inaccuracies
- 37% - Incorrect modifiers
- 35% - Failure to meet submission deadlines
- 34% - Patient information inaccuracy
- 33% - Missing or inaccurate claim data
- 33% - Not enough staff to keep up
- 27% - Formulary changes
- 27% - Changing policies
- 26% - Procedure changes
- 22% - Improperly bundled services
- 19% - Service not covered
Conclusion
With all of these health insurance claim denial statistics above, you can see that the situation needs some improvements. Healthcare organizations need to reduce the amount of denied claims and modify their claim resubmission process.
There are five things you can do to reduce the amount of denied claims…
- Determine the root causes of denials.
- Prioritize remediation based on what action steps have the greatest impact.
- Consolidate revenue cycle technology with a single vendor that covers everything “end to end”.
- Use advanced analytics software and AI to your advantage.
- Choose the right partner.
Etactics has been a clearinghouse for over 20 years. This means we have over two decades of experience with managing claims and preventing denials. We offer end-to-end advanced revenue cycle management solutions such as IntelliClaim and AppealsPlus.
With these tools, Etactics helps providers understand their denied claims and begin to prevent them from happening strategically. These tools help providers address their toughest revenue cycle challenges so your organization can remain focused on your patients. After all, patient care is what matters most.
Emphasize your product's unique features or benefits to differentiate it from competitors
In nec dictum adipiscing pharetra enim etiam scelerisque dolor purus ipsum egestas cursus vulputate arcu egestas ut eu sed mollis consectetur mattis pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus mauris aliquam ornare nisl purus at ipsum nulla accumsan consectetur vestibulum suspendisse aliquam condimentum scelerisque lacinia pellentesque vestibulum condimentum turpis ligula pharetra dictum sapien facilisis sapien at sagittis et cursus congue.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Incorporate statistics or specific numbers to highlight the effectiveness or popularity of your offering
Convallis pellentesque ullamcorper sapien sed tristique fermentum proin amet quam tincidunt feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.

Use time-sensitive language to encourage immediate action, such as "Limited Time Offer
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Address customer pain points directly by showing how your product solves their problems
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Vel etiam vel amet aenean eget in habitasse nunc duis tellus sem turpis risus aliquam ac volutpat tellus eu faucibus ullamcorper.
Tailor titles to your ideal customer segment using phrases like "Designed for Busy Professionals
Sed pretium id nibh id sit felis vitae volutpat volutpat adipiscing at sodales neque lectus mi phasellus commodo at elit suspendisse ornare faucibus lectus purus viverra in nec aliquet commodo et sed sed nisi tempor mi pellentesque arcu viverra pretium duis enim vulputate dignissim etiam ultrices vitae neque urna proin nibh diam turpis augue lacus.




