The 5 Main Causes of Burnout in Healthcare
Reducing burnout in healthcare is important for both workers and patients. It’s hard to tend to clients if you’re mentally exhausted. The only way to combat this growing issue is by understanding how it occurs in the first place.

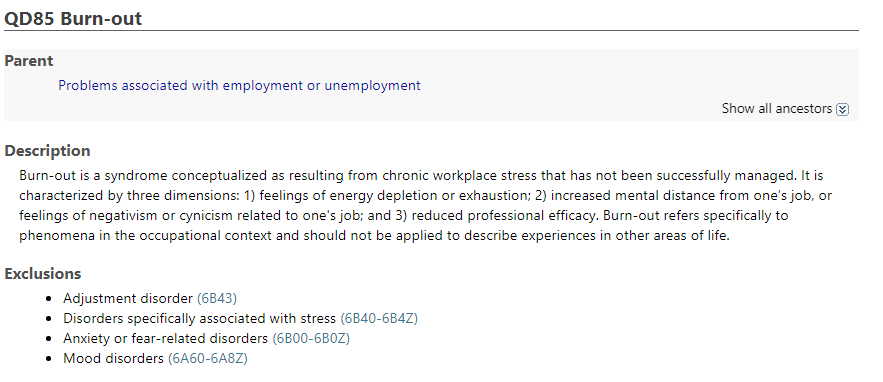
The World Health Organization (WHO) is addressing mental health in the workplace. It’s reclassifying burnout in the 11th Revision of the International Classification of Diseases (ICD-11).
The current definition of burnout in ICD-10 is the “state of vital exhaustion.” It doesn’t mention its relation to occupation.
The new description in ICD-11 is “a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed.” Although the new description isn’t releasing until January 1, 2022, this is a huge change.
In the new revision, this classification’s recognized as an occupational phenomenon, not a medical condition. They’ve done this to emphasize that it’s a result of stress caused at work. It’s not to refer to areas in life outside of the professional world.
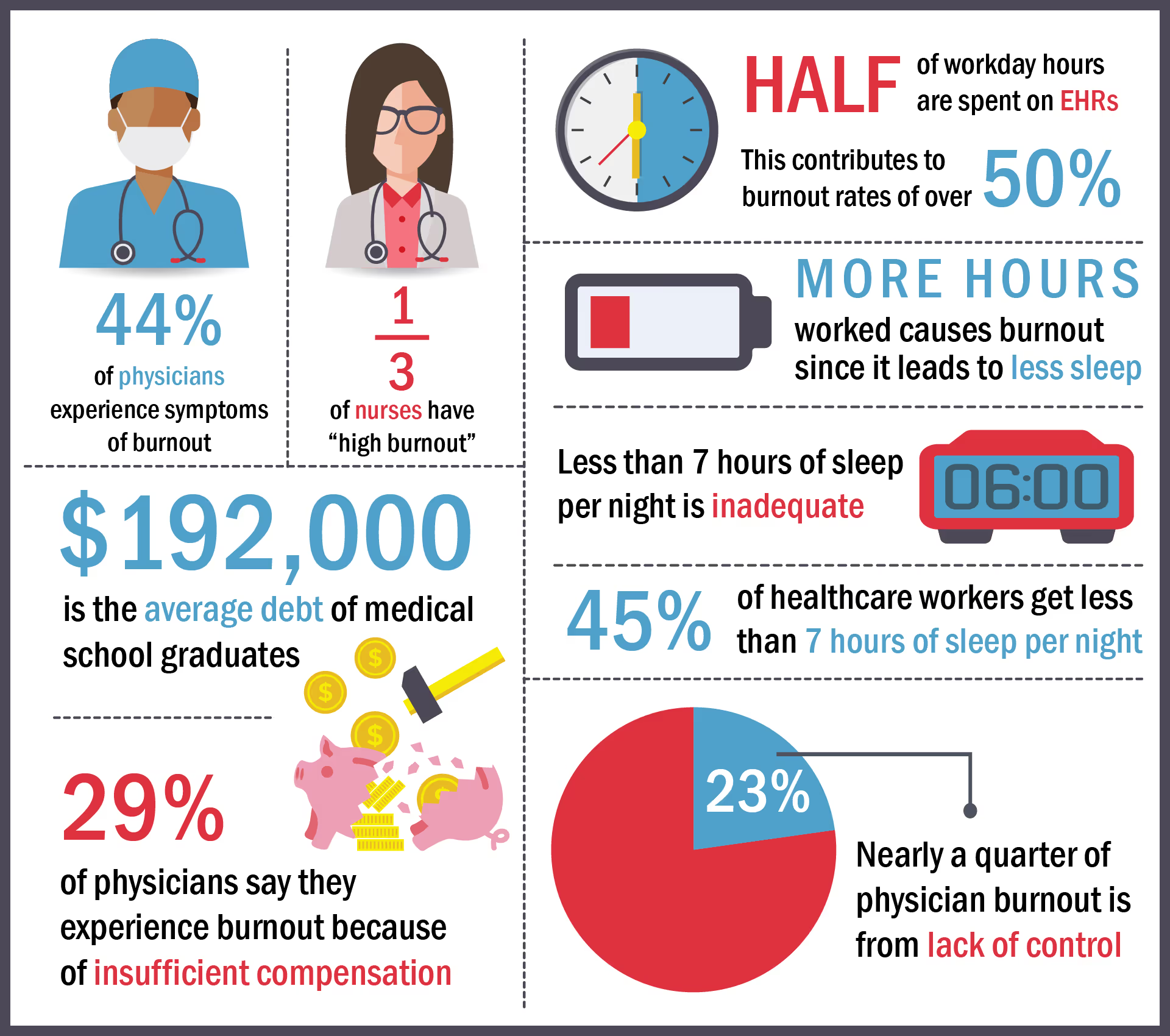
A recent report found that 44% of US clinicians have symptoms of burnout. This condition happens to them more often than any other occupation. What’s worse is the majority of them don’t try to reduce it or plan to seek help. Emergency workers have it even worse because of the chaotic nature of their workload.
Reducing burnout in healthcare is important for both workers and patients. It’s hard to tend to clients if you’re mentally exhausted. The only way to combat this growing issue is by understanding how it occurs…
Clunky Workflow Epidemic
The purpose of electronic health records (EHR) is to make administrative operations more efficient. Yet many of these systems have a poor user interface (UI) which causes the opposite effect.
The situation’s so bad right now that clinicians spend over half of their workday on EHR tasks, including more time after work hours.
Instead of spending more time with patients, these clunky UIs require the majority of their attention. The result is physicians feeling as though their neglecting their clients. Poorly designed EHRs contribute to burnout rates of over 50%.
Solutions to this cumbersome EHR epidemic are in development. Many startups are working toward creating AI technologies that reduce administrative tasks across the board. They intend to provide physicians with more time so that they can focus more on patient care.
Overwhelming Amount of New Tech
As I hinted in the section above, the healthcare industry is expanding its technologies. But, in some cases, workers struggle to keep up. While the intent is for these technologies to reduce stress in the long run, they may actually add to it.
Medical workers already have limited time. But new technologies demand more time for training, integration, and ensuring proper cybersecurity.
New tech must be easy to understand and use so that doctors are more likely to adopt them. Optimization is necessary to support clinicians in providing better patient care.
Integrating new tools in areas that already cause burnout, such as EHRs, may be an incentive for doctors to adopt other technologies. If the tools reduce workloads in one area, workers will have more time and patience to use them in other areas, too.
Long Hours and Sleep Deprivation
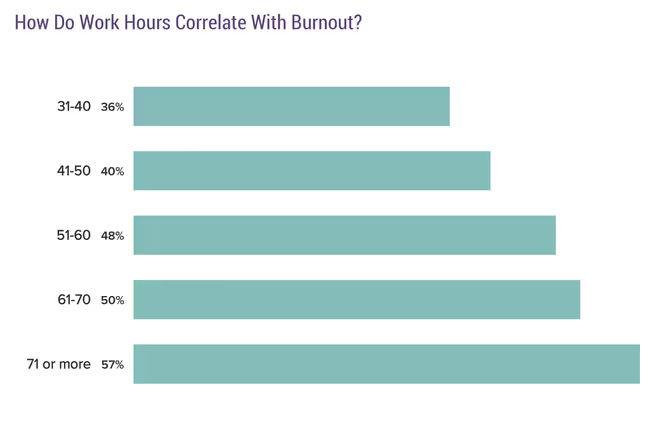
Healthcare employees often work long hours, including after hours, to keep up with administrative tasks. People who work more hours and earn more for their positions often get less sleep.
The recommended amount of sleep is around 7 hours per night, which less than this is inadequate. You already know what happens when you don’t get enough sleep. It negatively affects your...
- Mood
- Attention span
- Memory
Researchers analyzed data to assess sleep duration of American adults. Self-reports from 150,000 respondents showed that 45% of healthcare workers get inadequate sleep. Ironically, one of the industries that require the most attention to detail faces sleep deprivation.
Working non-traditional hours such as night shifts can also cause burnout. Out of everyone in the medical field, nurses have these hours most often. It just so happens that one-third of nurses also report high-levels of exhaustion.
Every person has a “normal” sleep-wake cycle that matches the time of day, that’s called a circadian rhythm. This rhythm is most sensitive to light. When people work at night, the lack of sunlight tricks the brain into releasing melatonin. This hormone influences the body to sleep. So while working a night shift, medical employees also disrupt their biological rhythm. This disruption accelerates mental exhaustion.
Mental fatigue leads to stress which also disrupts sleep patterns. This conundrum creates a never-ending negative cycle that causes burnout.
Financial Stress and Student Debt
Student debt also contributes to burnout in healthcare. Medical school is expensive, forcing students to take out higher loans than average. Over 75% of graduates are in debt when they begin working, which isn’t a surprise. More shockingly, medical students face an average debt of $192,000.
This debt burden puts extreme financial pressure on new physicians. This leads to doctors working more to pay back their debt. But the more they work, the more stressed they become.
A Medscape report found that 29% of physicians credit insufficient compensation to their exhaustion. They have less money for lifestyle spending and retirement savings since they spend so much on student loans.
Also, malpractice costs can cause further financial strain on medical professionals. Expensive liability insurance and costs associated with malpractice claims stress doctors out. Not to mention the potential of facing a lawsuit at any given moment.
The threat of a malpractice lawsuit can cause extreme levels of stress on physicians.
Overall Loss of Control
Doctor’s don’t have as much decision-making power as they used to in the workplace. Their increased loss in autonomy is the cause of almost one-quarter of cases involving burnout in healthcare.
First, physicians used to be the primary decision-makers of patient care. Now, the responsibilities also fall on hospital administrators, lawyers, and business-people. This shift stems from an industry-wide adjustment in priorities and financial pressures.
Second, health insurance companies dictate patient care based on what services they’ll cover. This siphons even more autonomy away from doctors.
Third, although helpful, technologies that replace the need for doctors leave them feeling discredited. They’re forced to give up some control over their practice since these new solutions assist with decisions.
Conclusion
Burnout negatively affects both healthcare workers and patients. Stressful situations lead to poor decision-making that bleeds into patient treatment.
Also, it impacts on your staff. As it widdles down their patience, they’ll end up leaving their jobs which makes yours much harder.
Organizations need to understand why this condition occurs. Only then will they be able to reduce it. Until that happens, medical workers will struggle to perform better or stay at their job.
Emphasize your product's unique features or benefits to differentiate it from competitors
In nec dictum adipiscing pharetra enim etiam scelerisque dolor purus ipsum egestas cursus vulputate arcu egestas ut eu sed mollis consectetur mattis pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus mauris aliquam ornare nisl purus at ipsum nulla accumsan consectetur vestibulum suspendisse aliquam condimentum scelerisque lacinia pellentesque vestibulum condimentum turpis ligula pharetra dictum sapien facilisis sapien at sagittis et cursus congue.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Incorporate statistics or specific numbers to highlight the effectiveness or popularity of your offering
Convallis pellentesque ullamcorper sapien sed tristique fermentum proin amet quam tincidunt feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.

Use time-sensitive language to encourage immediate action, such as "Limited Time Offer
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Address customer pain points directly by showing how your product solves their problems
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Vel etiam vel amet aenean eget in habitasse nunc duis tellus sem turpis risus aliquam ac volutpat tellus eu faucibus ullamcorper.
Tailor titles to your ideal customer segment using phrases like "Designed for Busy Professionals
Sed pretium id nibh id sit felis vitae volutpat volutpat adipiscing at sodales neque lectus mi phasellus commodo at elit suspendisse ornare faucibus lectus purus viverra in nec aliquet commodo et sed sed nisi tempor mi pellentesque arcu viverra pretium duis enim vulputate dignissim etiam ultrices vitae neque urna proin nibh diam turpis augue lacus.




