All Too Common Challenges in Caring for the Elderly
For this blog post we’ve aggregated statistics and best practices from various scientific sources. That way, you can get all of the trending information regarding this topic all in one place.

Of adults who live to age 65 or older, 70% develop needs for long-term services and support. Relying on care services could look different depending on the individual’s situation.
Some people end up receiving help from their family who takes over as their health support system. Others have home health caregivers who visit them at their residence to provide services. And the obvious option is that the elderly use nursing homes or other care facilities.
Difficulties exist across all types of services. Of course, these can vary depending on where and who the patient receives services from. For example, challenges for families are different from other care since they provide more personal support.
But no matter where the help is from, there are challenges in caring for the elderly. For this blog post we’ve aggregated statistics and best practices from various scientific sources. That way, you can get all of the trending information regarding this topic all in one place.
Family Members
Financial Burden
Nursing home costs could fall on the family if the patient can’t afford it. But long-term care facilities are a huge expense. People also don’t want to see their loved ones end up in a nursing home.
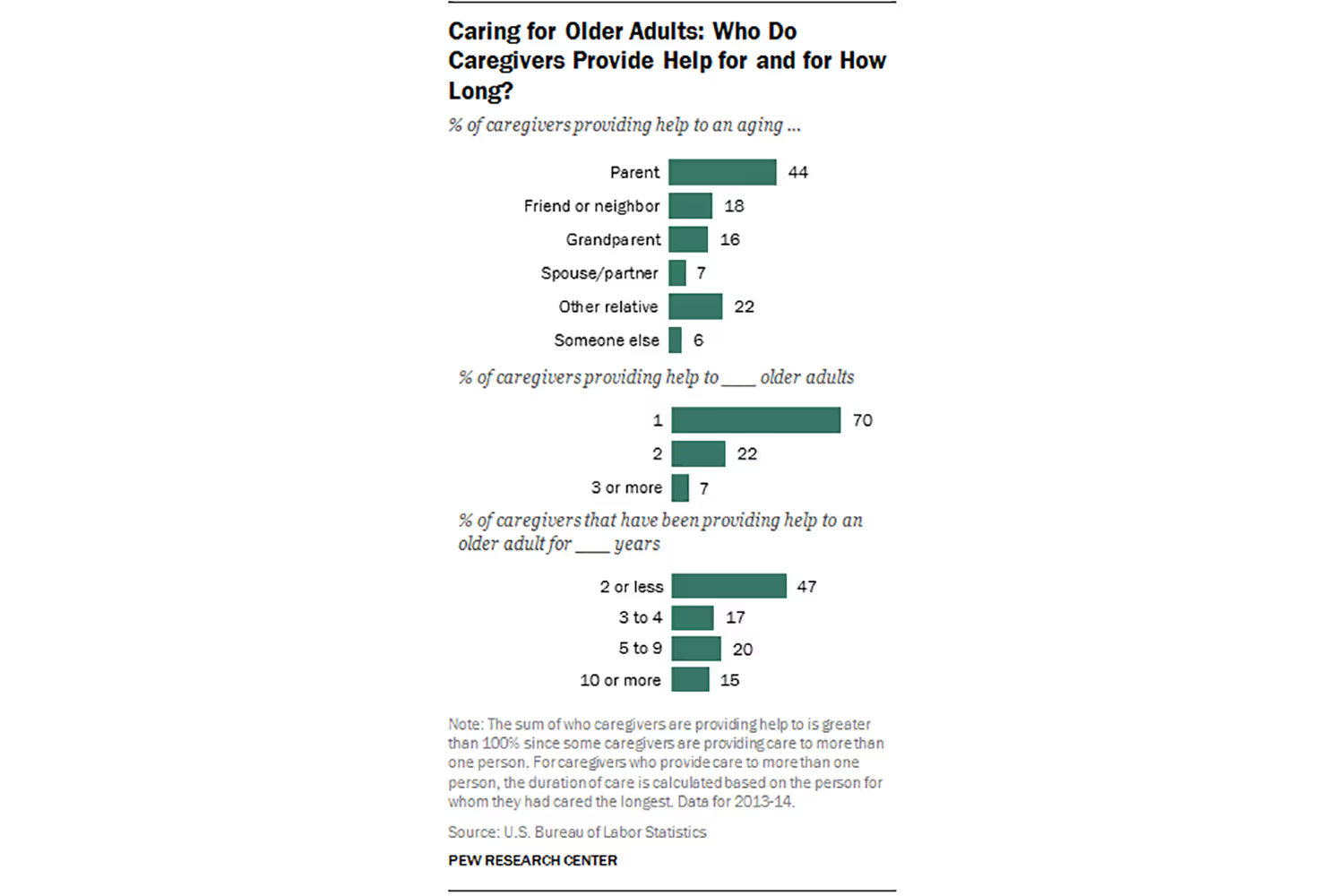
Because of this, family members may step up instead. But they aren’t likely to get paid for caring for the elderly relative. This means that costs still need to come out of their pocket. As of 2015, there were 40.4 million unpaid caregivers in the US for adults 65 and older. Nine out of ten were providing care for an aging relative.
Providing unpaid help while caring for the elderly also takes time away from paid work opportunities. If someone has to dedicate more time to help a relative, it can cut into the time they previously spent at a paid job.
Physical Demands
Depending on the patient’s condition, it can be physically demanding for a family member to help them. They won’t likely have the necessary equipment to support them unless they paid for it, of course.
Elderly adults may need help showering, getting to the bathroom, or walking up and down the stairs. Doing these without the right equipment can pose safety risks for the patient and family member. Physically supporting an adult with mobility trouble is difficult without the right tools, such as rails or ramps. This brings me to the next challenge.
Accessibility
Older adults will likely rely on accessible equipment at some point in their life. This varies depending on the patient’s condition. Some accessible options include:
- Walker
- Wheelchair
- Ramps
- Railings
- Shower chair
- Adjustable bed
- Elevator or stairlift
The list goes on. These tools aren’t as easy to get for a patient’s home, while they are more available in long-term health facilities. They also add more in-home costs that can get difficult to manage.

Lacking this equipment makes it harder for families to provide care. It’s also discouraging for the patient to have physical limitations. With these frustrations, families can’t easily help their loved ones. And in turn, it creates physical demands like I already mentioned.
Time Commitment
Family members spend over 24 hours per week caring for their loved ones. This doesn’t necessarily include time spent on caregiving duties, which many families say is over 40 hours each week.
If they don’t live together, there’s also driving time to consider. If the older adult is less independent then it could mean cutting out time from the supporter’s personal life. Scaling back on work, missing out on personal activities, and losing time with other relatives can become an emotional burden.
Emotional Stress
Spending more time with the patient also leads to isolation for the caregiver. By dedicating so much time to an older relative, they miss out on interactions with their other loved ones.
The time commitment isn’t the only cause for emotional stress. Everything I’ve mentioned so far can contribute to it. Financial stressors of meeting the person’s needs and making their environment physically safe demands a lot of a person.
Not to mention that it’s difficult to see loved ones become unwell. Relatives, whether they’re the primary caregivers or not, worry about the individual. It has impacts on their emotional health especially stress and anxiety, worry or fear, and sadness or depression.

Changing Relationship Dynamics
Relationships can change as relatives start helping their loved ones. When people have less independence and privacy, they can start to feel embarrassed or frustrated. This can make them avoid asking for help to maintain their dignity or so they don’t feel like a burden.
In one situation, an 89-year-old woman toned down her condition to maintain a sense of who she was. She said that she wouldn’t complain about her pain to her sons, even though she was in pain. Older people want to keep a sense of dignity and remain independent as long as possible. They don’t want the family to get involved if they can avoid it since they know it will change the dynamics of their life.
Dynamics will also change with the caregiver and their outside relationships. Spending more time caring for the elderly means less time with others such as a spouse, children, or friends. It can be difficult to start tending to a parent while also raising children.
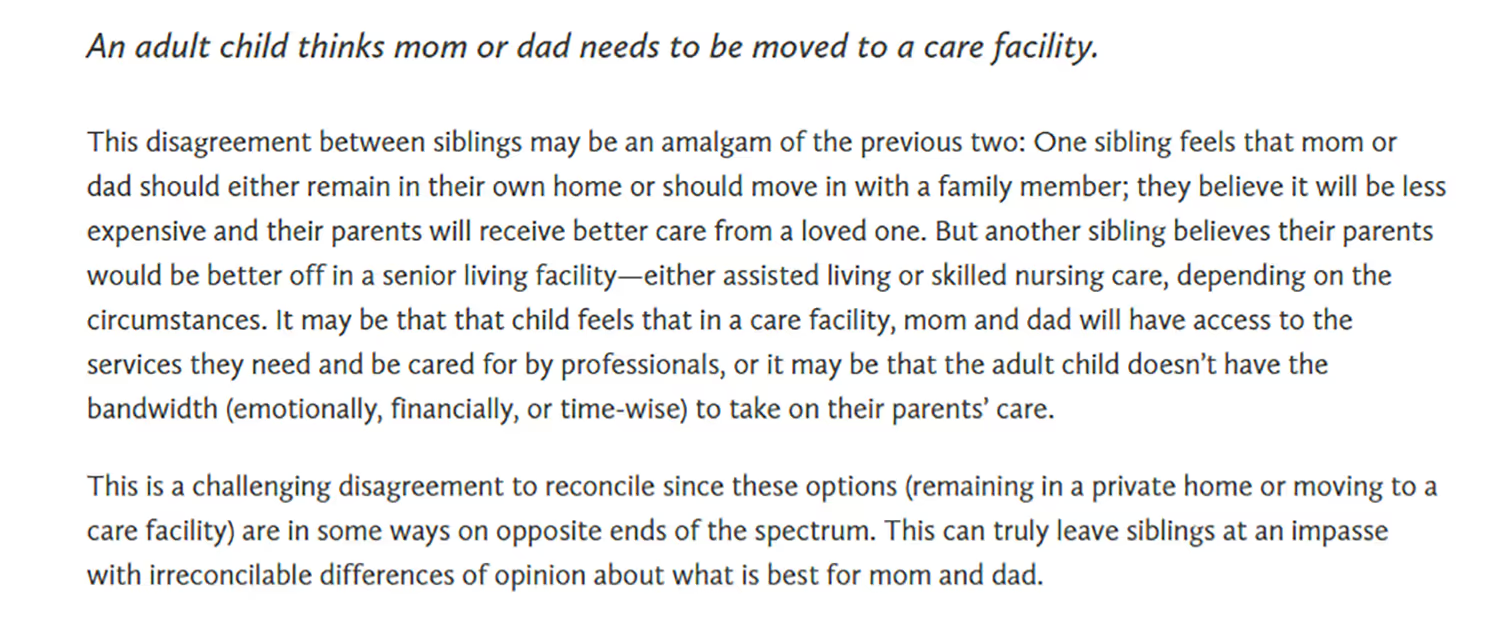
And different relatives may want different things for the older family member. This is especially true for siblings who need to make decisions for their parents.
Having other siblings to help can ease some burdens, but disagreements can occur regarding their healthcare. Some may think that a nursing home is the best option, while another sibling thinks it’s best to keep the parent home and have everyone contribute. This creates family tension that can result in rivalry if it’s not dealt with.
Home Health Workers
Time Constraints
Even though these professionals provide services in the home similar to family, they differ in the services they provide. Many home health workers have professional training and do this for their careers.
But this means they can’t dedicate as much of their time to a patient as families might be able to. Because they deal with multiple clients, they only have so much time they can dedicate to the person. One nurse reports seeing six patients each day, but sometimes more if the team needs additional help.
This leaves a two-hour block when the patient can expect the visit. These are routine since they set their schedules for when they come to provide services.
As a result, the individual may not be getting some care during times that they need it. The worker also won’t be able to see everything that goes on in the day to know how else the patient may need help.
Safety Concerns
Going into a stranger’s home is always a safety concern. A health worker never knows what they might walk into. These people often work alone, increasing their risks. If a patient becomes agitated, it’s difficult to manage a violent situation when there’s no one else to help.
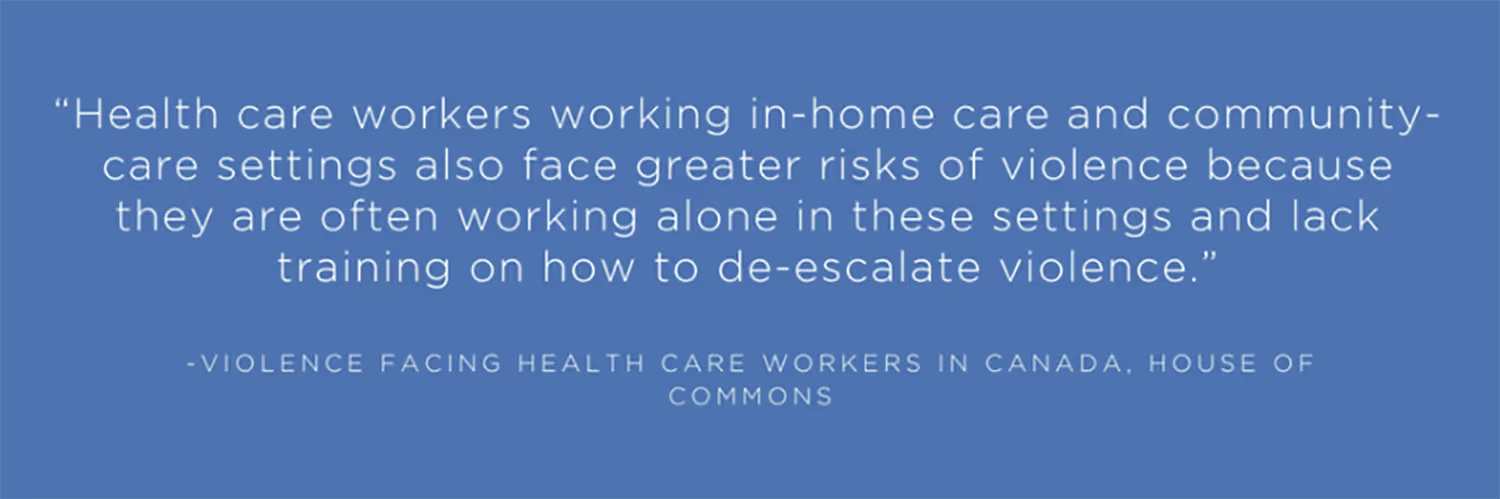
Believe it or not, workplace violence is a common problem in the health industry, and the likelihood only increases for in-home health. In the US, workers in this environment are the most susceptible to verbal abuse, aggression, threats, and sexual harassment. Up to 61% of home health workers experience this violence.
If the home is unsanitary, there are also health hazards for workers and patients. A home health worker gets exposed to diseases and it’s unsafe to provide services when the environment isn’t clean.
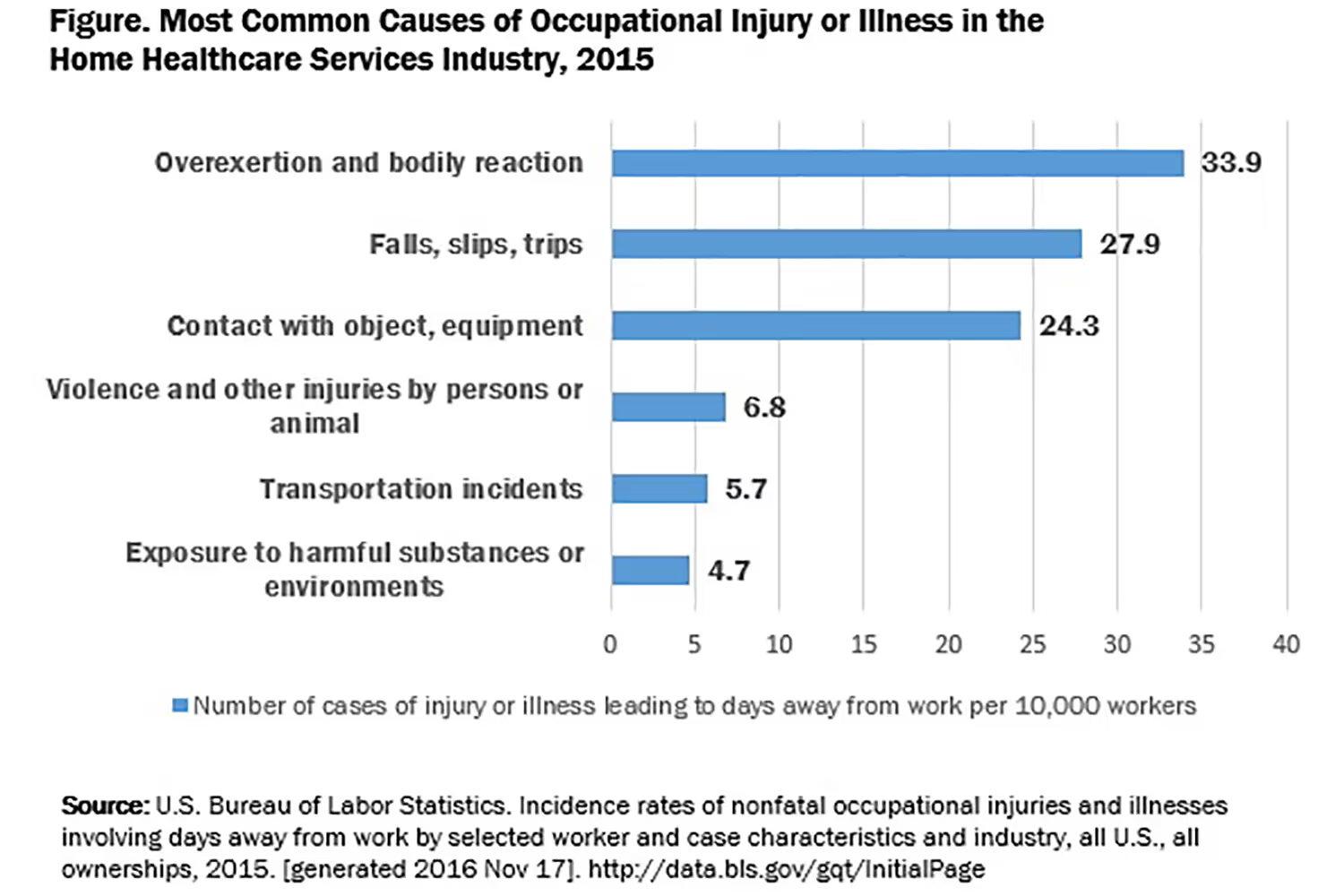
Inadequate Equipment
The lack of proper equipment is also a challenge for home health workers. They see the same issues that a family provider would face. When the home doesn’t have proper accessibility, it becomes much harder to provide the best help. It can even cause occupational injury such as overexertion.
There is also a limit of health supplies.
Since home health workers have to bring all of their supplies with them, they may run into a situation where they don’t have the material they need. This makes it much harder than if they were in a health facility where supplies are always on hand.
Limited Support
Since these workers are on their own when giving care, they lack support. They can’t easily ask another staff member for help like they would be able to do in a residential home. If something goes wrong, there isn’t another nurse to assist and there’s no medical staff on site.
With a large aging population, more people will rely on home health services. As workers need to take on more patients to keep up with demand, it’s an even bigger challenge to get support from other staff.
There may also be less support from the family. Since the patient has home health assistance, relatives may think they don’t need to help as much. Or they begin expecting more from the worker. But there’s only so much that these professionals can do with limited time with a patient.
And in some cases, the patient has no family hence why they need home health in the first place. This means the individual is relying solely on the several hours that the home health worker can provide.
Care Facilities
Growing Aging Population
I’ve mentioned already that there’s a growing aging population. By 2050, the population aged 65 and older could reach 83.7 million. This is nearly double from 2012.
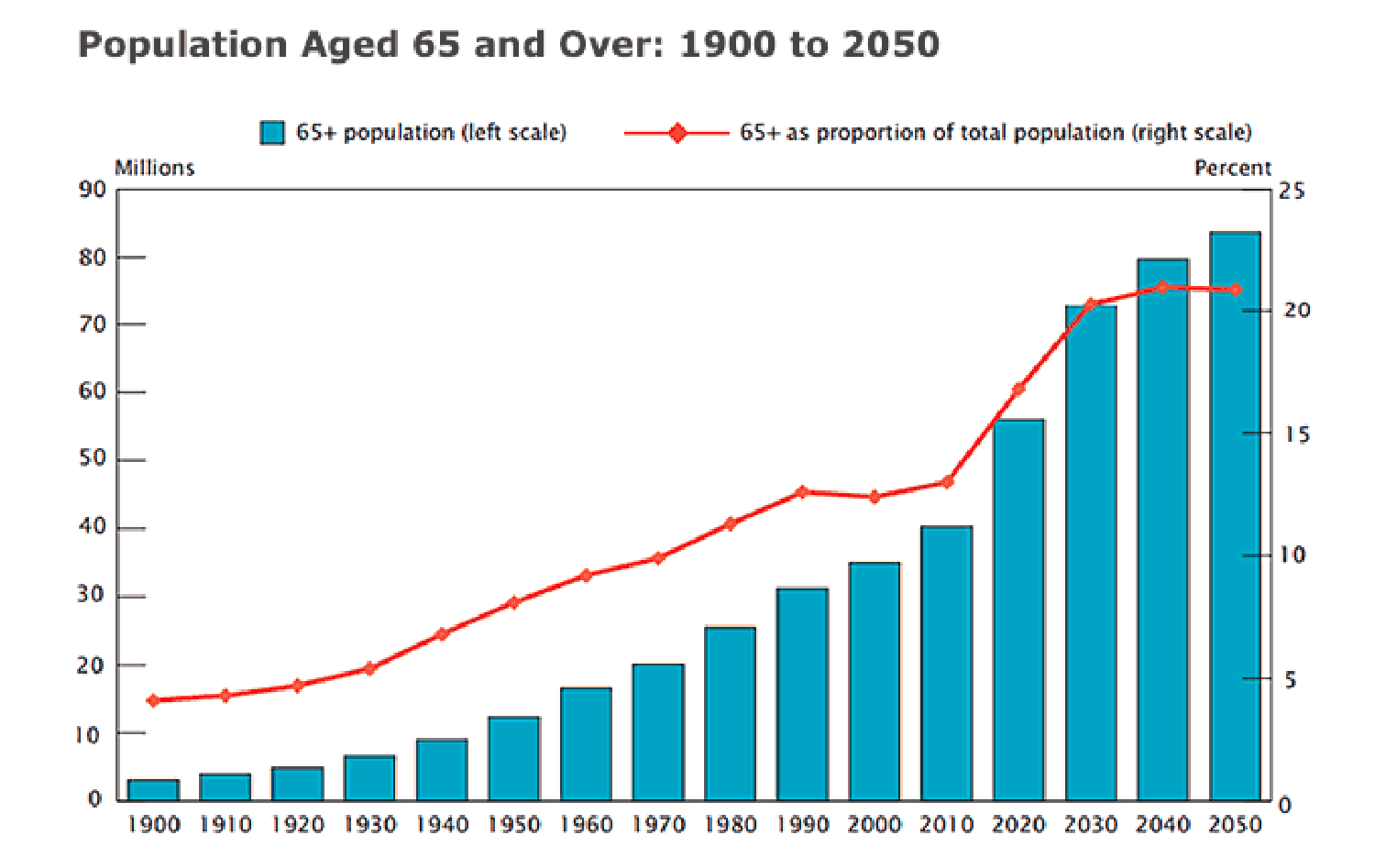
Because of the large population and that people are living longer, there’s a strain on long-term facilities. More patients will need more funding, staff, and supplies. But all of these have their challenges.
Costs and Financing
Nursing home costs have a negative financial impact on patients and facilities. Medicaid is the primary payer for these facilities but only covers 70% to 80% of the actual cost of nursing home care. The funding gap leads to inadequate budgets and operating losses for nursing home providers.
The burden on Medicaid will likely increase significantly over the next several decades. There’s a rising cost of care, a large aging population, and a higher demand for long-term services. Since the financial pressure is going to be difficult for Medicaid and payers to handle, the state budgets will carry the burden.
This has led to the consideration of incentives that will improve the market for purchasing long-term care insurance. This would appeal to informal caregivers like friends and family, and also reduce some of the public sector’s burdens.
Staff Shortages
More residents will rely on more staff. But unfortunately, there’s already a shortage of health workers. Last year alone, the shortage in at least one staff category of nursing homes increased from 19.9% in May to 22.8% in December.
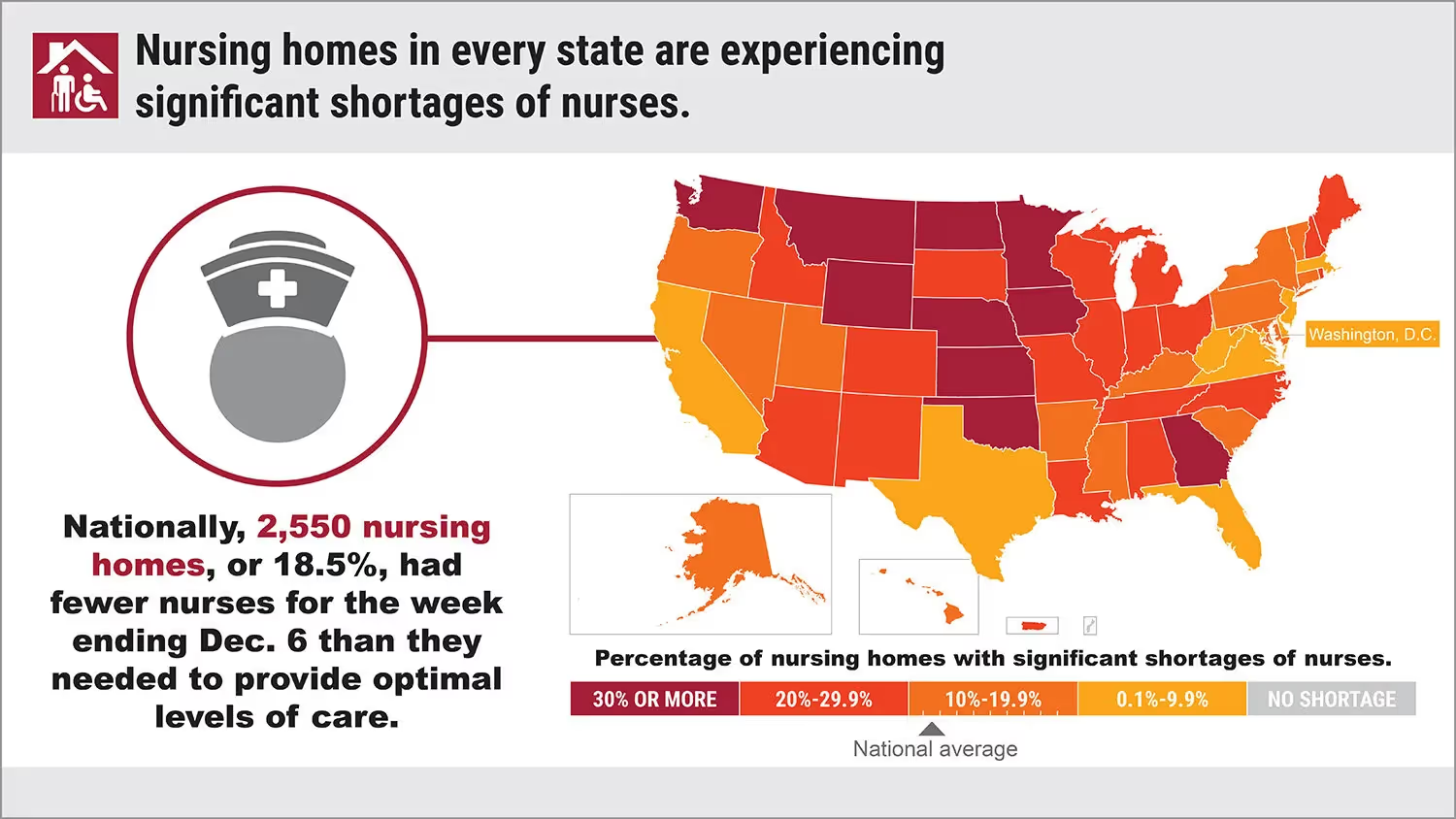
Since the number of employees is already lacking, it will be difficult for the industry to keep up with so many new residents. Facilities may need to turn away residents or deal with understaffing which can cause burnout.
Even worse, when there are more patients than workers to keep up with them, the quality of services can decrease.
Quality of Care Standards
It’s more important than ever that facilities provide high-quality care. This can be difficult with more patients, but it’s necessary so that people will still utilize these long-term options. The quality of nursing homes has mostly improved over time.
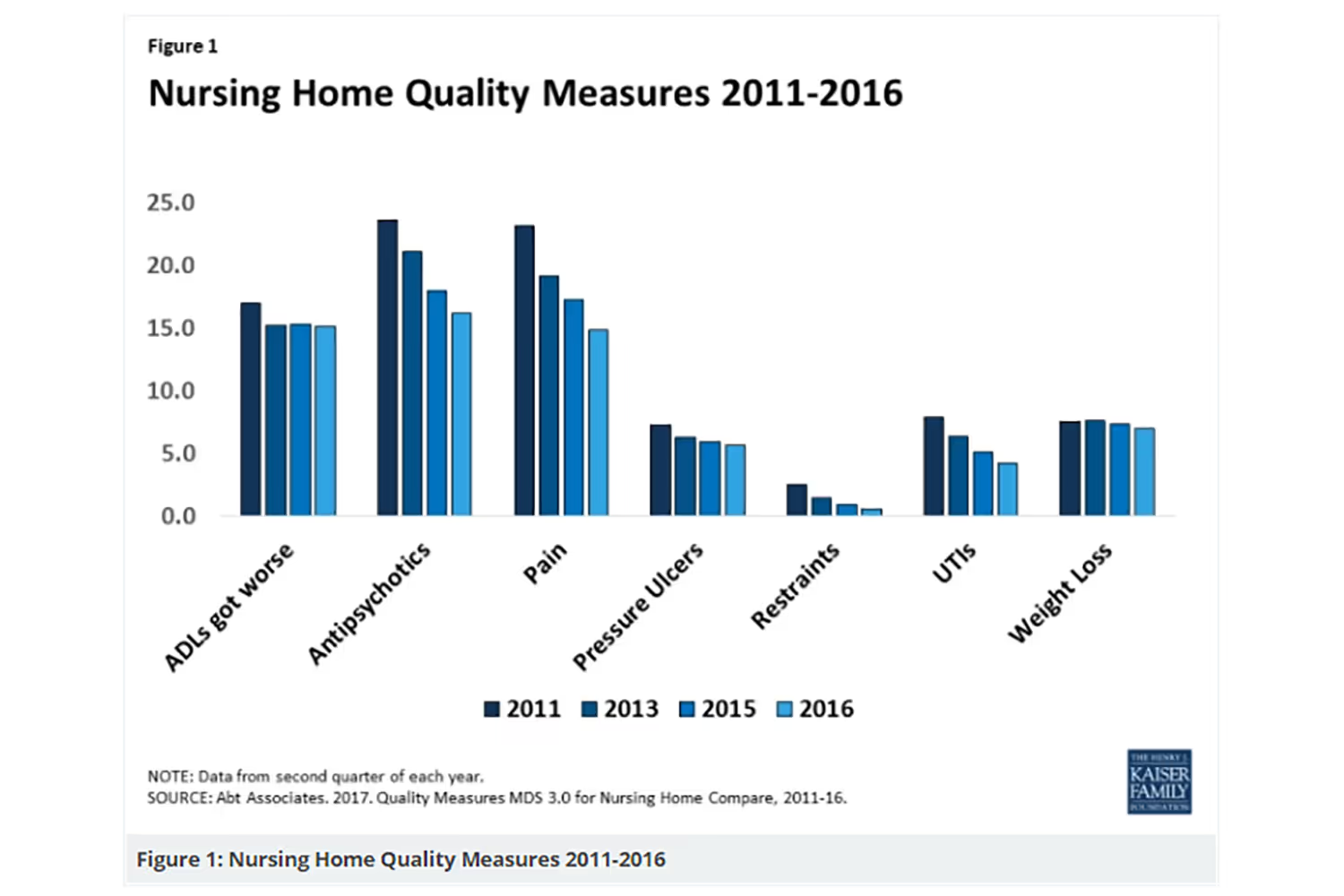
But many still fail to meet federal quality standards. In 2015, around 93% received at least one inspection deficiency citation. 21% had deficiencies for serious quality violations.
Since it costs so much for patients to stay in these facilities, they and their families expect high-quality care. If the nursing home doesn’t meet the standards, it can drive clients away and cause a bad reputation.
Disease Management
Part of quality standards includes disease management. Overcrowded homes can increase the spread of disease transmission. Patients are already vulnerable and at risk for infections, so it’s important to limit this spread.
During the COVID-19 pandemic, residential facilities saw large outbreaks. 30% of the US deaths were among residents and staff of these homes. This was because of their vulnerability to disease and how easy it could spread between people living close together.
As a result, nursing homes must have necessary precautions for handling illness spread. Anything contagious poses a risk to residents, so staff must find ways for maintaining transmission.
The elderly also have the most chronic diseases of any other age group. The risk of these conditions increases with age. Around 85% of these older adults have at least one chronic disease, while 60% have at least two.
Tending to many people with multiple illnesses relies on a structured schedule. When they need more medications, it takes consistency and attention from everyone on the team. This way they receive their proper treatment.
Conclusion
As more people get older, there’s a larger population that will rely on health services. This could come from family, home health workers, or a residential facility.
Challenges in caring for the elderly arise in all of these options. While difficulties can vary, each has similarities. Not addressing the concerns can cause other problems to arise as well.
This is why it’s necessary to manage challenges before the health industry gets more overwhelmed by the large older population. Mitigating struggles will make it easier to provide care and keep patients healthy and satisfied with services. It even eases the lives of their families as well.
Emphasize your product's unique features or benefits to differentiate it from competitors
In nec dictum adipiscing pharetra enim etiam scelerisque dolor purus ipsum egestas cursus vulputate arcu egestas ut eu sed mollis consectetur mattis pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus mauris aliquam ornare nisl purus at ipsum nulla accumsan consectetur vestibulum suspendisse aliquam condimentum scelerisque lacinia pellentesque vestibulum condimentum turpis ligula pharetra dictum sapien facilisis sapien at sagittis et cursus congue.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Incorporate statistics or specific numbers to highlight the effectiveness or popularity of your offering
Convallis pellentesque ullamcorper sapien sed tristique fermentum proin amet quam tincidunt feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.

Use time-sensitive language to encourage immediate action, such as "Limited Time Offer
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Address customer pain points directly by showing how your product solves their problems
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Vel etiam vel amet aenean eget in habitasse nunc duis tellus sem turpis risus aliquam ac volutpat tellus eu faucibus ullamcorper.
Tailor titles to your ideal customer segment using phrases like "Designed for Busy Professionals
Sed pretium id nibh id sit felis vitae volutpat volutpat adipiscing at sodales neque lectus mi phasellus commodo at elit suspendisse ornare faucibus lectus purus viverra in nec aliquet commodo et sed sed nisi tempor mi pellentesque arcu viverra pretium duis enim vulputate dignissim etiam ultrices vitae neque urna proin nibh diam turpis augue lacus.


.avif)

