40+ Shocking Workplace Violence in Healthcare Statistics
Healthcare is one of the leading industries where workplace violence occurs. Here are over 40 statistics that explain why that is.

A survey found that over 70% of nurses worry about workplace violence. Of the respondents, 20% said that this was extreme worry.
Workplace violence in healthcare often occurs from the extreme behavior of patients. The situations are unpredictable because diagnoses can vary and don’t always result in aggressive behavior.

Different factors cause patient agitation such as pain, devastating prognosis, and disease progression. This leads to them acting out, resulting in assault and attacks against healthcare workers.
When healthcare workers face these incidents, they’re more likely to have emotional distress that causes them to leave their jobs. This has major turnover costs for the organization. And that’s not even including the costs of those who miss work due to being victims of this violence.
These are situations that should always get addressed in the health industry. Incidents justify a report to management and law enforcement. Yet it’s difficult to address these because many still don’t get reported.
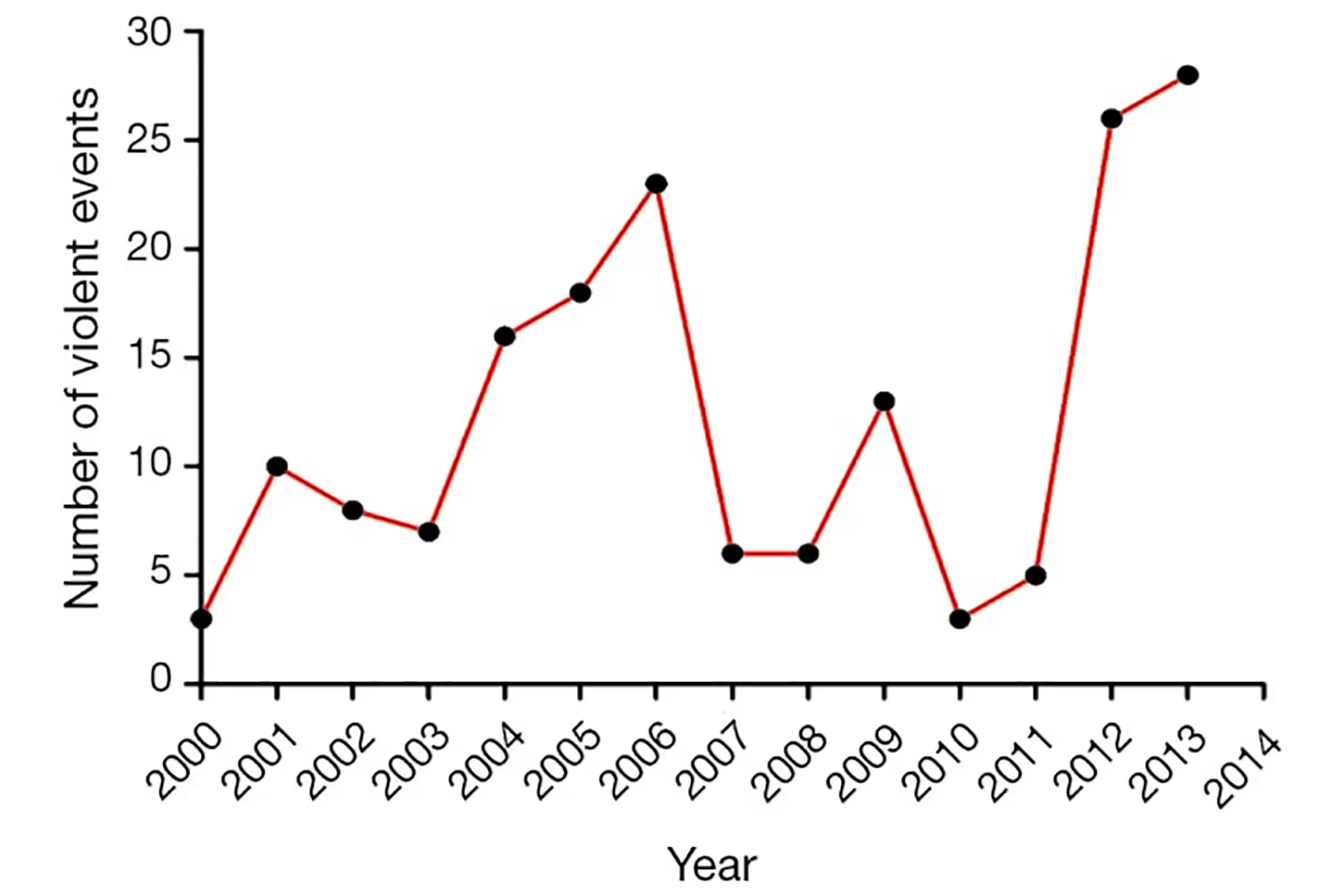
A Growing Issue in Healthcare
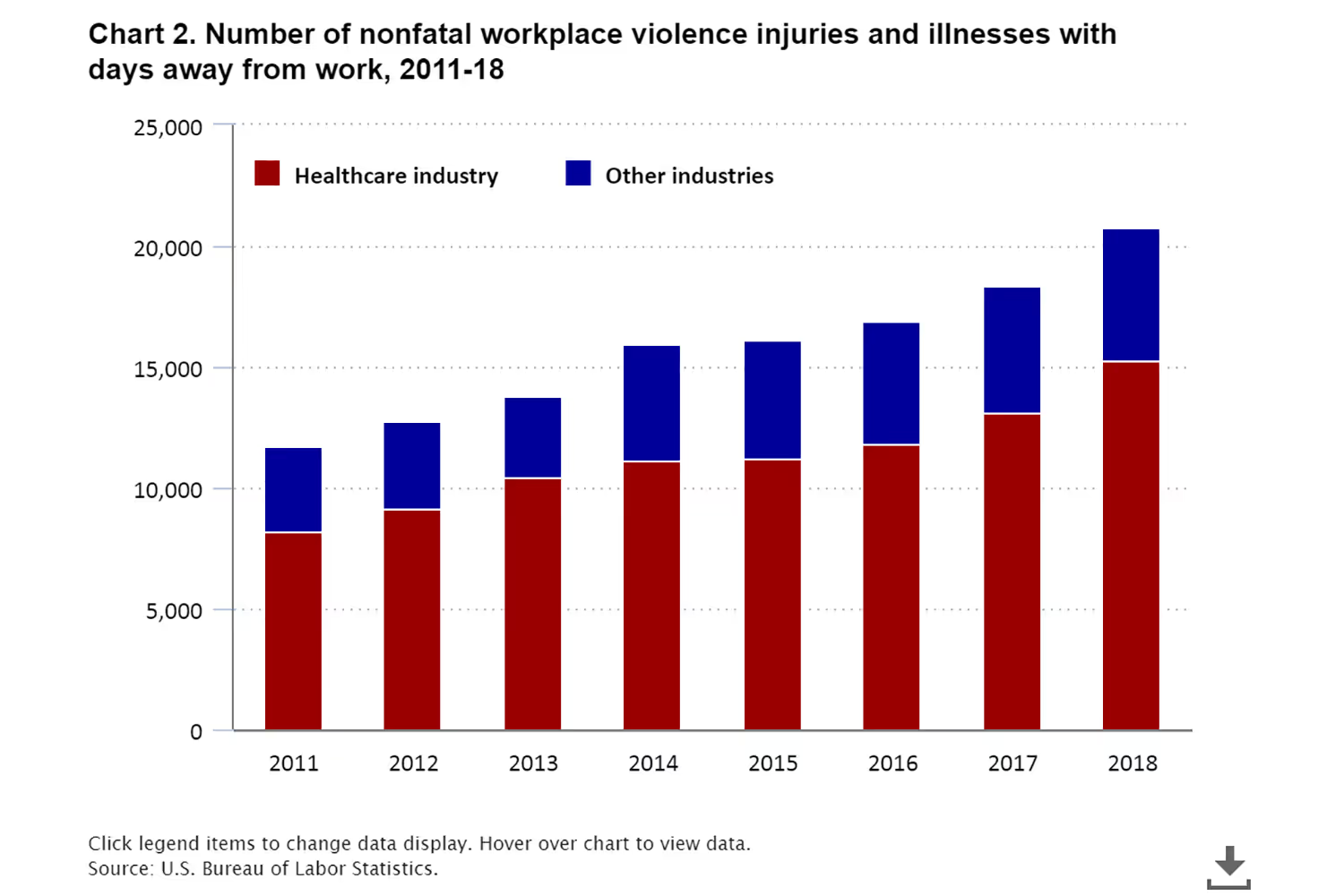
Workplace violence in healthcare isn’t slowing down. Even though it’s a known problem, it still occurs more frequently today than it did in the past decade.
Interventions are necessary to slow these rates so that healthcare workers (HCWs) will stay in their positions. This will also help protect patients - those harming, and others who may experience impact from an incident. So how common is it?
- 7 of 10 physicians said that violence in emergency departments is increasing. (American College of Emergency Physicians)
- 80% said that the incidents harmed patient care. (American College of Emergency Physicians)
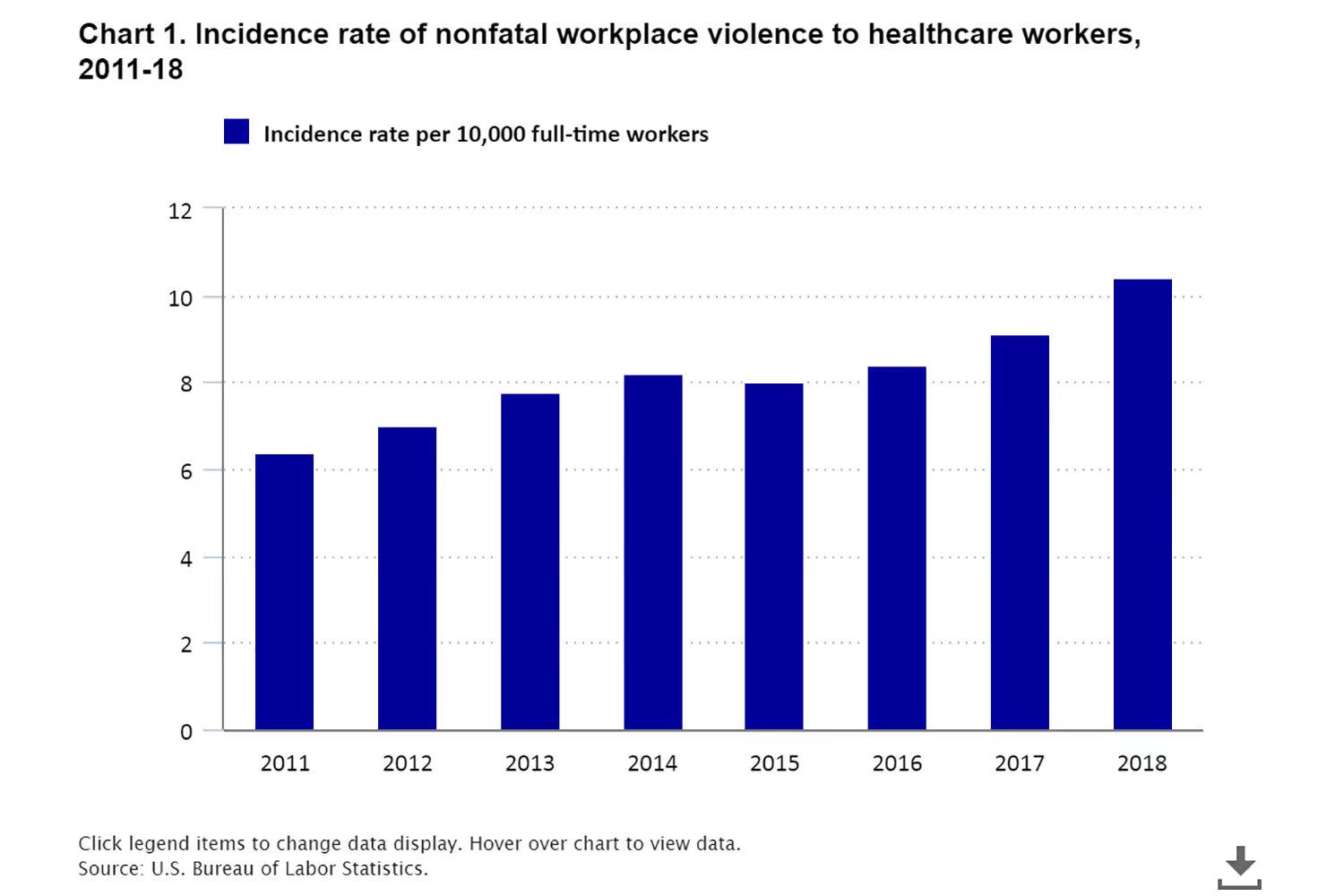
- In 2018, the incidence rate of nonfatal workplace violence to healthcare workers was 10.4 per 10,000 workers. This increased from the 2011 rate of 6.4 per 10,000. The rate for all industries was only 2.1 in 2018. (US Bureau of Labor Statistics)
- Health workers have a 20% higher chance of being the victim of workplace violence than workers in other industries. (Sentinel Event Alert)
Costly Situations
The more often these issues occur in a hospital, the more costly it is for the organization. They’ll incur costs from the harm itself and the turnover that it results in.
Injuries that occur from this lead to people missing work. And in some cases, it requires treatment that the hospital is responsible for through worker’s compensation.
Witnessing incidents or being the victim themselves also causes emotional exhaustion and burnout. Eventually, this burnout leads staff to leave positions in the health field. This turnover causes hospitals to lose money from restaffing. They’ll either be paying other employees overtime and bonuses to fill in, or they have to spend more money on recruiting.
- 13% of days out of work were due to workplace violence. (American Nurses Association)
- HCWs who experience these incidents use around 112.8 hours of sick, disability, and leave time annually. This costs hospitals $53.7 million per year. (Milliman Research Report)
- One study found that of the injuries at a large US hospital system, 54 resulted in average costs of $3,138 per incident. (911Cellular)
- Exposure to these situations increases depression, anxiety, and emotional stress for employees. This results in HCW turnover, and turnover of a registered nurse costs hospitals $5.2M to $8.1M. (Nursing Solutions, Inc)
Rates by Department
Different departments experience higher rates of violence. Some high-risk areas are emergency departments, geriatrics, and behavioral health units. This is due to the stress and agitation that patients feel here. With more discomfort, there’s a greater chance that they act out.
Studies show that higher levels of stress hormones can lead to aggression. These hormones lead to a vicious cycle where escalated aggressive behavior is difficult to stop once it starts.
This explains why nonviolent people can become violent in stressful situations.
As a result of this, patients who get agitated or experience increased high stress are likely to lash out. And certain departments have more frequent stressful situations than others.
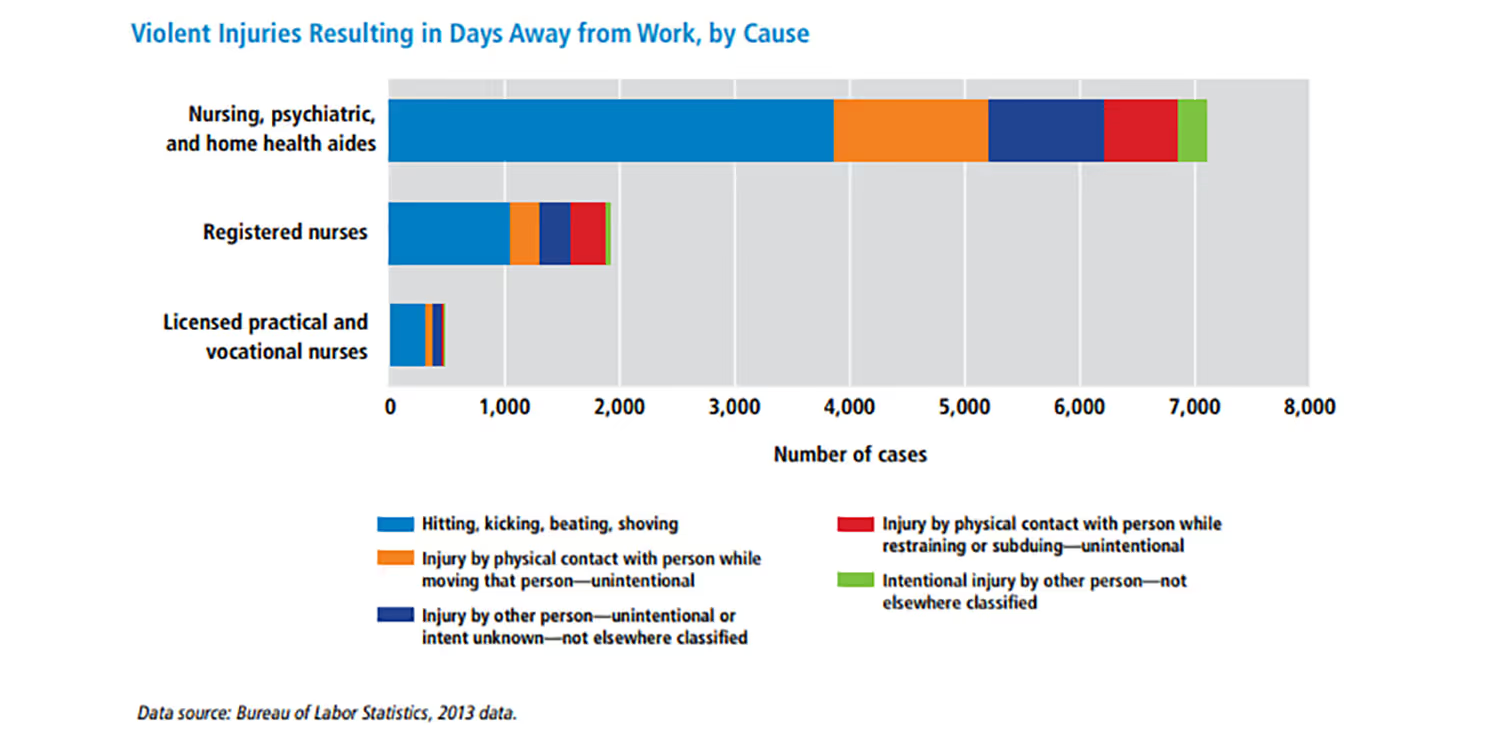
- Psychiatric aides experienced the highest rate of violent injuries that resulted in days away from work in 2013. This was around 590 injuries per 10,000 full-time workers, more than 10 times higher than the next most prevalent group. Nursing assistants experienced around 5 per 10,000 full-time workers. (OSHA)
- Between 24% to 80% of HCWs in acute psychiatric units experienced some form of assault from patients during their careers. Verbal assaults affect 46-78.6%, threats affect 43-78.6%, and sexual harassments affect 9.5-37.2%. (NCBI)
- Close to 50% of emergency doctors experienced assault, and 70% of emergency nurses reported getting hit or kicked while working. (AAMC)
- Nurses in the emergency department have the most worry. Over 60% say they felt “very worried” or “extremely worried” about violence on the job. (NCBI)
- Nursing and residential care facilities had the highest prevalence of nonfatal work violence in 2015. This rate was 6.8 per 100 full-time employees, the highest of all medical settings. (ACP Hospitalist)
Incidents Don't Get Reported
Incidents don’t always get reported, whether it’s victims who don’t report to their managers or the hospital which doesn’t inform law enforcement. If the hospital doesn’t take action or communicate with legal authorities, victims will have less of a reason to report them to their managers. They’ll feel little sense in filing an incident if nothing gets done about it.
Others have the mentality that these situations are a normal part of their job. This culture of expecting these to happen contributes to a lack of reporting. Even though workplace violence has become a more frequent problem, it isn’t new that people expect it.
- Around three-quarters of 25,000 assaults occur each year. But only 30% of nurses and 26% of emergency department physicians report the violence. (AJMC)
- A survey of 4,738 Minnesota nurses found that 69% of physical assaults and 71% of non-physical assaults got reported to a manager. (OSHA)
- Around 77% of nurses agreed or strongly agreed that they expected assault as a consequence of their job. (Minnesota Nurses’ Study)
Experiences in Different Countries
Workplace violence in healthcare is an international problem. Each country experiences different rates and instances of this harm. Across the globe, health organizations need to address this consistent issue. That way, both workers and patients will feel safe and protected.
- In the USA, 70-74% of workplace assaults are in healthcare. (NCBI)
- In Italy, 50% of nurses experienced verbal assault, 11% experienced physical violence, and 4% experienced a threat with a weapon. (FNOMCeO)
- Over 30 hospitals in South Africa reported serious security incidents in just 5 months during 2019. (MedicalBrief)
- Almost 37% of emergency medical services personnel experience physical, verbal, or cultural workplace violence in Iran. (ResearchGate)
- 96% of surveyed Chinese hospitals experienced violence in 2012. As of 2014, the prevalence of verbal abuse or physical injuries at work was over 70% for physicians. (NCBI)
- 91% of primary care physicians in Germany experienced aggressive behavior at some point during their jobs. 73% were in the previous year, and 23% included severe aggression. (PubMed)
- There were 56,435 physical assaults on the UK’s NHS staff in 2016-2017, compared to 51,447 in 2015-2016. (HSJ Guides)
Conclusion
Workplace violence is a real issue across the globe, especially in healthcare. It’s common for patients to get agitated in a medical setting if they are unwell, causing them to act out.
These instances are so common that workers even expect them to occur. Yet it still leaves them distressed to the point that they leave their jobs. Since they don’t always report these situations, it’s unlikely for the scenarios to change, hence why they’re still increasing.
And employees aren’t the only ones at risk for negative impacts even though the violence is against them. It also disrupts care, harms patients, and leads to large expenses for hospitals.
Because of this, organizations must address these issues so that they’ll occur less frequently. That way, staff will feel safer and more inclined to stay. It will also improve patient safety and comfort so that they have higher satisfaction at the hospital.
Emphasize your product's unique features or benefits to differentiate it from competitors
In nec dictum adipiscing pharetra enim etiam scelerisque dolor purus ipsum egestas cursus vulputate arcu egestas ut eu sed mollis consectetur mattis pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus mauris aliquam ornare nisl purus at ipsum nulla accumsan consectetur vestibulum suspendisse aliquam condimentum scelerisque lacinia pellentesque vestibulum condimentum turpis ligula pharetra dictum sapien facilisis sapien at sagittis et cursus congue.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Incorporate statistics or specific numbers to highlight the effectiveness or popularity of your offering
Convallis pellentesque ullamcorper sapien sed tristique fermentum proin amet quam tincidunt feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.

Use time-sensitive language to encourage immediate action, such as "Limited Time Offer
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Address customer pain points directly by showing how your product solves their problems
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Vel etiam vel amet aenean eget in habitasse nunc duis tellus sem turpis risus aliquam ac volutpat tellus eu faucibus ullamcorper.
Tailor titles to your ideal customer segment using phrases like "Designed for Busy Professionals
Sed pretium id nibh id sit felis vitae volutpat volutpat adipiscing at sodales neque lectus mi phasellus commodo at elit suspendisse ornare faucibus lectus purus viverra in nec aliquet commodo et sed sed nisi tempor mi pellentesque arcu viverra pretium duis enim vulputate dignissim etiam ultrices vitae neque urna proin nibh diam turpis augue lacus.


.avif)

