50+ Shocking Physician Burnout Statistics You'll Never Believe
Healthcare professionals increasingly face depression, high stress, and emotional exhaustion. Each of these severe ailments leads to burnout. Here are over 50 shocking physician burnout statistics you’ll never believe.

We’re drowning.
Around one in four Americans suffer from diagnosable psychological disorders each year. These disorders affect everyone around us and bleed into our professional life.
The state of mental health is so bad right now that companion chatbots exist to work as therapists that are available around the clock.
It doesn’t matter what industry you serve, you can still get overwhelmed. But out of all the professions out there, physicians and medical professionals have it the worst.
Although they may seem invincible, they’re susceptible to the same illnesses that they’re treating patients for and psychological disorders know no boundaries. The nature of their profession requires them to help people in their weakest states but that’s near impossible if they’re not the best version of themselves.
Healthcare professionals increasingly face depression, high stress, and emotional exhaustion. Each of these severe ailments leads to burnout. To pile on, many of them aren’t receiving the help that they need even though they’re showing signs of suffering.
Here are 25 shocking physician burnout statistics you’ll never believe.
42% of Physicians Experience Burnout in 2021
(Mayo Clinic)
A survey of physicians found that 42% experienced symptoms of burnout. The five specialties that ranked the highest were different in 2021 due to the pandemic. This year, the lineup includes critical care at 51% (7% more than last year), Rheumatology at 50% (4% more than last year), and infectious diseases at 49% (4% more than last year.
NEW: NEARLY HALF OF GENERATION X PHYSICIANS SAID THEY FELT BURNED OUT
(The Wall Street Journal)
A survey of more than 15,000 physicians was conducted in 2020. The statistic above is quite startling when compared with the fact that 39% of baby boomers and 38% of millennials said they felt burnt out.
96% of Medical Professionals Agree that Burnout is an Issue
(NEJM Catalyst)
Not only do doctors recognize this issue, but their executives and leaders agree. 31% recognize that it’s a moderate problem, and 65% believe it’s a serious problem. More clinical leaders see it as a serious problem than executives.
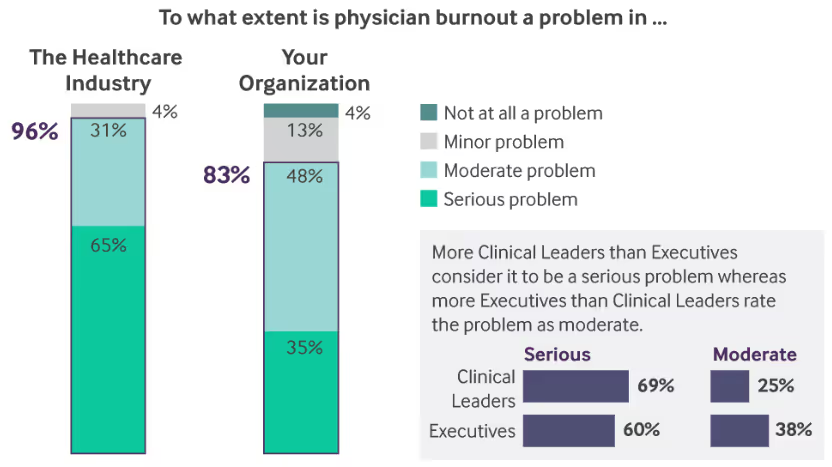
This is actually a pretty positive statistic. The less time it takes for C-Suite executives to understand this problem, the sooner change will happen.
60% OF RESPONDENTS SAID “TOO MANY BUREAUCRATIC TASKS” CAUSES BURNOUT
(LeverageRx)
Bureaucratic tasks include charting and paperwork. This chews up lots of time for physicians and prevents them from seeing more patients. 50% of physicians work at least 60 hours a week, with a good chunk of the time allotted to paperwork.
42% OF PHYSICIANS ARE RELUCTANT TO SEEK MENTAL HEALTH TREATMENT
(Psychiatry Advisor)
Doctors fear their job security or loss of their practice if word got out that they needed help themselves. If you think about it, this mindset makes sense. Their job is to take care of patients. If word gets out that they need help too they might think they’ll lose trust in their clients.
Almost half of all physicians think they can handle their struggles without professional help. But keeping depressive thoughts and feelings bottled up only worsens the issue.
43% OF MEDICAL PROFESSIONALS ISOLATED THEMSELVES TO DEAL WITH BURNOUT IN 2021
(Medscape)
While many doctors don’t seek professional mental health treatment, they may still try coping. These coping methods aren’t always healthy, though. Of those physicians who experience burnout, 4 in 10 try to cope by isolating themselves from others.
Everyone deals with their mental health in different ways but no one should weather the storm alone.
26% OF MEDICAL PROFESSIONALS DRANK ALCOHOL TO DEAL WITH BURNOUT IN 2021
(Medscape)
Many people self medicate with alcohol. They try to numb their feelings, destress, or forget the things they have seen. This is true for doctors since one in four physicians will drink to cope with burnout. This number has increased since 2020 when 24% of physicians admitted to drinking as a coping mechanism.
40% of Doctors With Burnout Say They Lack Resources
(athenaInsight)
Physicians’ levels of productivity directly affects their psychological state. If doctors are more productive in their work, they may feel less burnout. This can happen from many different factors. More productivity leads to more pay, they may have better interactions with patients, and they may feel more successful.
But lacking appropriate resources to be productive causes burnout. 40% credit their burnout to a lack of tools and resources that are necessary to provide high-quality patient care.
51% OF FEMALE PHYSICIANS EXPERIENCE BURNOUT COMPARED TO 36% OF MEN
(MedScape)
Female doctors have consistently reported higher rates of burnout compared to male doctors throughout the last few decades. 2021 showed a greater disparity compared to normal. A psychiatrist at the Montefiore Medical Center attributed this due to the impact of COVID-19 on family units. It is well known that women assume more responsibilities in the home compared to men, so women also assume more pressure when children are learning digitally.
SUICIDE DEATHS ARE ROUGHLY 250 to 400% HIGHER AMONGST FEMALE PHYSICIANS COMPARED TO FEMALES IN OTHER OCCUPATIONS
(eMedCert)
This makes a lot of sense when you take some of the statistics above into consideration. Doctors in general have higher rates of suicide compared to the general public. Plus female doctors have higher rates compared to male doctors. So when you combine those facts, it is not surprising that female doctors are 4X more likely to commit suicide compared to women in other industries.
94% of Female Physicians with a Diagnosis Don’t Disclose It
(Science Direct)
A study of female physicians found that only 6% of those with a mental health diagnosis reported it to their state licensing board. The women responded that they’d never want a diagnosis on their records for fear of stigma.

53% OF DOCTORS WITH DEPRESSION SAID IT AFFECTED THEIR WORK IN 2021
(Advisory Board)
Only 47% of depressed doctors said that their mental state doesn’t interfere with patient interactions. But 35% experience more irritation with patients. Another 26% had less motivation to be careful with patient note-taking. Even worse, 14% made mistakes that they wouldn’t normally make.
21% of PHYSICIANS EXPERIENCING BURNOUT SAID IT WAS BECAUSE OF COVID-19.
(MedScape)
The conditions of the pandemic have increased the rate of burnout. From the difficult conditions, constant stress, long hours, to losing so many patients to the virus, many factors of the pandemic took a toll on doctors.
37% OF PHYSICIANS SAID THAT TOO MANY HOURS AT WORK CONTRIBUTES TO BURNOUT
(MedScape)
The main causes of burnout remain consistent with reports from previous years. The pandemic has amplified the situation, but it was a problem even before the chaos of the pandemic.
72% OF PHYSICIANS HAVE EXPERIENCED A REDUCTION OF INCOME DUE TO COVID-19
(NIHCM Foundation)
Pay and income is one of the top reasons why physicians experienced burnout. Because of the 2020 pandemic conditions, the situation got worse. Nearly 3 out of 4 physicians had a pay reduction while simultaneously working extra hours.
Average Medical School Debt is $190,000 - $206,000
(Student Loan Planner)
Medical school is expensive. Doctors may have high-paying salaries, but the cost of loan repayment increases burnout and stress levels.
As of 2017, the average medical school debt was $190,000 per student. Debt averages were even higher at $206,000 for private medical school graduates. Even with a high salary, this debt is difficult to pay off.
Their debts place more financial burden on medical students than any other cohort.
Medical Students Experience 15-30% Higher Depression
(US News & World Report)
Medical school is stressful, time-consuming, and costly. Medical students are at a much higher risk than most people to face mental health issues. This demographics rate of depression is 15-30% higher than the general population.
45% of Resident Physicians Experience Burnout
(JAMA Network)
Residency is a stage of graduate medical school. Even before they’re practicing doctors, they face unhealthy levels of stress.
One survey found that on average, 45% of resident physicians experience burnout. This ranged from 29.2%-63.8%. The prevalence of career choice regret was between 7.4%-32.7%.
28% of Resident Physicians Experience Major Depression
(ACGME)
During training, 28% of resident physicians experience major depressive episodes. But only 7-8% of similarly-aged individuals in the general US population come close to experiencing these severe breakdowns.
Over 50% of doctors work 50-80 hours per week
(Pacific Companies)
Most physicians work 51-60 hours per week, but this only accounts for 26% of physicians. Another quarter work 60-80 hours, so a majority work between 50-80 hours. According to the Bureau of Labor Statistics, most Americans work an average of 34.4 hours per week.
Working more hours contributes to a higher frequency of stress, burnout, and depression.
54% of Doctors Say EHRs Decrease Professional Satisfaction
(Health Populi)
Doctors have higher satisfaction when they spend more time with patients. But they spend more than half of their workdays on EHRs, taking time away from patient care. These lengthy times spent on EHRs reduce their satisfaction.
Doctors Need Over 50% More Time With Patients
(AHRQ)
Doctors report feelings of stress due to time pressures at work. They have limited time with patients, especially due to administrative tasks.
One-third of doctors say that they need more than 50% more time for patient care functions. That would be all the time currently spent in EHR systems.
One in Five Doctors Plan to Reduce Work Time
(Healthcare Drive)
Burnout, stress, and depression are lowering physicians’ work-life satisfaction. Almost 20% of physicians surveyed said they would likely cut their work hours in the next year.
More than one quarter said that they were likely to leave their practice in the next two years. Some even reported that they planned to pursue a different career.
Physician Burnout Costs Up to $6.3 billion
(Annals of Internal Medicine)
This is a massive cost that healthcare faces. The true expense is between $2.6 billion and $6.3 billion per year. This is from the cost of recruitment and replacement of physicians when they leave their position or cut back their hours. Turnover is starting to become a problem.
The US Will See a Shortage of 122,000 Physicians by 2032
(AAMC)
There’s a growing, aging population in the US. More patients mean workloads for doctors. This doesn’t help the current issue that workloads cause burnout and stress. More patients will result in a large shortage of up to 122,000 physicians by 2032.
But increased workloads will increase exhaustion, so more physicians may leave positions. This would lead to an even greater shortage.
Doctors Experience 43% Emotional Exhaustion
(Verywell Health)
The proportion of doctors with “above threshold” levels of stress is 28% compared to the general population. This leads to higher emotional exhaustion rates: 24% for the general population, but 43% for doctors.
18% of Hospital Nurses Experience Depression
(Healthcare In America)
Burnout and emotional exhaustion causes depression in nurses, too. There are signs of depression in 18% of hospital nurses.
35%-54% OF NURSES AND PHYSICIANS EXPERIENCED BURNOUT IN 2019
(NIHCM Foundation)
Doctors aren’t the only healthcare professionals with high emotional fatigue. This ailment extends into nursing as well. As many as 54% of nurses and physicians reported emotional exhaustion scores that qualified as “high burnout.”
Half of Registered Nurses Consider Leaving the Profession
(RNnetwork)
No person should feel so stressed out in their career that they’re considering walking away from it forever. But various factors cause emotional exhaustion for nurses and they’re leading them to leave their profession. These include feeling overworked, too many administrative tasks, not enough time with patients, disrespect from administrators, and bullying or harassment from coworkers.
BETWEEN MARCH AND JULY OF 2020, 8% OF DOCTORS IN THE UNITED STATES PERMANENTLY CLOSED THEIR OFFICES
(NIHCM Foundation)
That 8% translates to an estimated 16,000 fewer private practices. If each practice had 10 employees, then 160,000 people became unemployed due to the closers. Also, if each practice served 1000 people a year, then 16 million people lost access to a doctor.
16-18% of Nurses and Physicians Meet Diagnostic Criteria of PTSD
(ACEP Now)
Post-traumatic stress disorder (PTSD) is a psychiatric disorder due to exposure to a traumatic event. Emergency health workers often experience these situations, so they’re at risk for PTSD. Studies show 18% of nurses and 16% of emergency physicians meet the criteria for a diagnosis of this disorder.
This rate is even higher for nurses in the intensive care unit since they deal with trauma incidents often.

300-400 Doctors Die by Suicide Each Year
(NPR)
Physicians commit suicide at rates of 28 to 40 per 100,000 people. This is over double the rate of the average American. Doctors are working in high-stress environments, which contributes to depressive disorder. These can then spiral into suicidal thoughts and attempts.
13% OF PHYSICIANS SAID THEY HAD SUICIDAL THOUGHTS BUT DID NOT ATTEMPT SUICIDE.
(Medscape)
In 2018, suicide was the tenth leading cause of death amongst civilians living in the United States. As horrific as this is, it gets worse. In 2021, 1% of doctors actually attempted suicide. An additional 5% of physicians, when asked if they had ever attempted suicide or thought of suicide, said that they preferred not to answer.
Female Doctors Have 250-400% Higher Rates of Suicide
(NCBI)
Death by suicide is already more common among health experts than any other profession. But this is even more likely for female physicians. According to a report from the American Foundation for Suicide Prevention, death by suicide is 250-400% more likely for female doctors due to stress and depression.
This is because they are more prone to and experience more negative outcomes from stress than other occupations.
THE SUICIDE RATE AMONGST PHYSICIANS IS 2X HIGHER THAN THE GENERAL PUBLIC
(NIHCM Foundation)
Due to the stress of the day-to-day routine, many doctors end up contemplating suicide. Doctors are so stressed out compared to the general population that they are twice as likely to think about suicide, and potentially attempt suicide as well.
Physician Suicide Rates Leads to 1 Million Lost Patients
(MD Magazine)
There is a huge, noticeable loss after physician suicide. This event not only affects friends and families but also patients. The average US doctor helps about 2,300 patients.
With up to 400 physician suicides per year, almost 1 million patients lose their medical expert.
Younger physicians are 200% more likely to experience symptoms of burnout
(AMA)
“Younger physicians” refers to doctors below the age of 55 years old. Although large, this group is much more likely to experience symptoms of burnout than older doctors. This could be because those experiencing this ailment at high levels more often switch their career paths.
Those who don’t experience a high level are more likely to stay in their positions and don’t feel the need to retire as early. Because of this, those older than 55 may have higher satisfaction.
But doctors who experience high burnout levels will switch careers well before they get to that age.
Those with children younger than 21 years old have 54% increased odds of burnout
(National Academy of Medicine)
Healthcare professionals who need to take care of children on top of their work responsibilities will experience more burnout. Work is already mentally and physically taxing, but when they return home, they have even more duties with their children.
It’s difficult to balance home and work life when the medical industry demands so much from its most skilled workers. This becomes a great emotional challenge to balance both, thus increasing chances to experience the ailment.
Only 67% would choose family medicine as their specialty again
(AAFP)
If you want to get into medicine you want to work in the smaller, family environment, right?
Well, over half of family physicians report symptoms of burnout, and only 29% report being happy at work. While 77% of family practitioners report they’d choose working in medicine again, only 67% of them would choose the family environment again.
More than half experience dissatisfaction with work-life integration
(Mayo Clinic)
In 2017, only 42.7% of medical professionals with symptoms of burnout reported satisfaction with their work-life integration.
This is a decrease from 2011, when satisfaction was 48.5%. Part of this is due to how much time physicians spend at work with long shifts, so they don’t have as much time for other activities in their personal lives.
Eventually, they may feel as if work is taking over their lives.
79% of those in primary care experience burnout
(InCrowd)
InCrowd conducted research in 2016 to develop their Physician Burnout Report. In 2019, they again asked this group for feedback on their job-related stress.
The most recent findings were similar to 2016 with 79% of primary care professionals reporting burnout. This is higher than the 54% of specialists who reported similar symptoms. But of both groups, more than one-third would not recommend their profession to a younger family member.
47% OF DOCTORS AT HEALTHCARE ORGANIZATIONS EXPERIENCE BURNOUT
(MedScape)
Healthcare organizations were among the top work locations where doctors burn out in 2021. Also in the top was outpatient clinics at 46%; office-based multispecialty group practices at 44%; and academic (nonhospital), research, military government at 42%.
10.5% make a “major medical error”
(ACP Hospitalist)
A survey found that over 50% of physicians experienced symptoms of burnout. Of the respondents, 10.5% reported that they had made a “major medical error” within only three months prior to the survey.
This could have been due to the 32.8% who had reported excessive fatigue. Experiencing high levels of exhaustion will cause difficulty focusing, which can in turn lead to mistakes.
Around 40 percent list hate regulatory and insurance requirements
(Physicians Foundation)
Health insurance doesn’t solely affect patients. There’s a lot of work that lands on the list of responsibilities for physicians as well.
A 2018 survey found that these insurance and regulatory requirements land on the list of tasks that healthcare professionals hate the most. One of the survey participants stated, “Retiring completely in one month. Mostly because of burnout. I find it stressful to adequately treat my patients and keep up with all insurance red tape and government regulations.”
Practice staff spend 12.5 hours weekly per physician handling quality measures
(Health Affairs)
As Medicare, Medicaid and private health insurance plans continue to expand, so too does the amount of quality measured put in place by the US government.
This requires coordinated effort between everyone within a practice, but the desk staff members end up doing the majority of the work. Most quality measure work requires data entry. Thus, staff members spend 10.2 hours per week entering in information.
67% feel that billing and coding in-house was responsible for stress and burnout in 2020
(Pain Physician Journal)
The healthcare industry, as a whole, faced a challenge in 2020 with the global COVID-19 pandemic. As a result, different stressors arose as leading causes to expert’s mental anguish.
Along with all of their other responsibilities, many facilities keep their billing and coding efforts in-house. Pairing that with the panic induced by a pandemic and many medical experts found themself stressed like never before.
Conversely, only 32% felt that outsourcing was responsible for their stress.
Trainees exposed to COVID-19 patients in 2020 reported significantly higher levels of stress
(PLOS ONE)
Being on the frontlines during a pandemic isn’t easy. Sure, that responsibility falls on any professional in healthcare as they’re the people we count on most when a health crisis happens.
However, that doesn’t mean they’re impervious to stress. Due to the nature of the crisis and the influx of COVID-19 patients, many healthcare organizations had to expedite the position of their trainees.
As a result, this group of professionals experienced severe stress.
Adequate personal protective equipment (PPE) throughout the COVID-19 pandemic protected against burnout
(National Institutes of Health)
In order to protect yourself and others, the majority of United State governments mandated that their citizens wear masks in public. The sheer panic of the pandemic brought forth many other shortages at grocery stores including; hand sanitizer, toilet paper, bread, etc.
Due to the demand created by both mandates and widespread panic there soon was a shortage of PPE.
As a result, healthcare workers experienced increased stress as some of them had to rely on homemade alternatives.
Conclusion
Many Americans suffer from mental health. But we tend to forget that this includes those professionals who take care of us.
Healthcare workers often suffer in silence. They fear the stigma surrounding mental illness, convincing themselves that seeking help would cost them their careers.
Factors within the medical space cause to high levels of burnout. This only increases the prevalence of mental illness.
Medical organizations need to recognize and end the factors not only leading to burnout but also its related disorders. They must work to reduce any negative thoughts related to talking about mental health. That way, professionals will seek help so they can then better care for their patients.
List of Sources:
- AAMC
- ACEP Now
- ACGME
- Advisory Board
- AHRQ
- Annals of Internal Medicine
- athenaInsight
- Health Populi
- Healthcare Dive
- Healthcare In America
- JAMA Network
- Mayo Clinic
- MD Magazine
- MedEd Web Solutions
- Medscape
- NCBI
- NEJM Catalyst
- NPR
- Pacific Companies
- Psychiatry Advisor
- RNnetwork
- Science Direct
- Student Loan Planner
- US News & World Report
- Verywell Health
- AMA
- National Academy of Medicine
- AAFP
- Mayo Clinc
- ACP Hospitalist
- The Physicians Foundation
- Health Affairs
- Pain Physician Journal
- PLOS ONE
- National Institutes of Health
Emphasize your product's unique features or benefits to differentiate it from competitors
In nec dictum adipiscing pharetra enim etiam scelerisque dolor purus ipsum egestas cursus vulputate arcu egestas ut eu sed mollis consectetur mattis pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus mauris aliquam ornare nisl purus at ipsum nulla accumsan consectetur vestibulum suspendisse aliquam condimentum scelerisque lacinia pellentesque vestibulum condimentum turpis ligula pharetra dictum sapien facilisis sapien at sagittis et cursus congue.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Incorporate statistics or specific numbers to highlight the effectiveness or popularity of your offering
Convallis pellentesque ullamcorper sapien sed tristique fermentum proin amet quam tincidunt feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.

Use time-sensitive language to encourage immediate action, such as "Limited Time Offer
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Address customer pain points directly by showing how your product solves their problems
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Vel etiam vel amet aenean eget in habitasse nunc duis tellus sem turpis risus aliquam ac volutpat tellus eu faucibus ullamcorper.
Tailor titles to your ideal customer segment using phrases like "Designed for Busy Professionals
Sed pretium id nibh id sit felis vitae volutpat volutpat adipiscing at sodales neque lectus mi phasellus commodo at elit suspendisse ornare faucibus lectus purus viverra in nec aliquet commodo et sed sed nisi tempor mi pellentesque arcu viverra pretium duis enim vulputate dignissim etiam ultrices vitae neque urna proin nibh diam turpis augue lacus.


.avif)

