Denial Code CO 18: A Comprehensive Guide
Denial code CO 18 is a common denial code. Here’s everything you need to know about it including what it is, what it’s common and how to overturn it.

One in every three hospitals reports that their denial rate is 10% or higher according to Harmony Healthcare.
A denial rate that high is what’s considered to be the “danger zone” when it comes to denials.
How have hospitals let their denial rates hit such alarming percentages?
Change Healthcare pinpoints the pandemic as the cause of these alarmingly high rates. According to its 2020 Denials Index report, denials rates had risen by 11% on average since the onset of COVID-19.
I know, so far all of the statistics I’ve thrown at you have been pretty negative.
The truth is, though, that there really shouldn’t be any reason why the claim denial landscape is so grim. You see, 8 out of every 10 denials are completely avoidable.

In other words, most healthcare organizations have the opportunity to collect on claims that insurance organizations didn’t initially accept…they’re just not doing it.
But, why would healthcare organizations be OK with leaving so much of their revenue on the table only to write it all off as losses at the end of the year?
It’s likely more of an internal knowledge and workflow problem. After all, when an insurance organization denies a claim its reasoning comes back as a code with not much more explanation behind it.
With over 20 years of experience as a clearinghouse provider, we help healthcare organizations manage their denials by making them more manageable with built-in workflows and translating insurance organizations.
Throughout those couple of decades, we’ve started to notice that certain denials tend to show their faces more often. As such, we feel that it’s important to help explain the relevance of the common denial codes that we see, how to avoid them and overturn them.
Denial code CO 18 is one such common denial code. Here’s everything you need to know about it including what it is, what it’s common and how to overturn it.
What is denial code CO 18?
Before trying to overturn any type of denial, you need to understand what it is.
Denial code CO 18 means, “exact duplicate claims or services.”
That’s great, but what is an exact duplicate claim? An exact duplicate means that the payer determined that the same claim was already submitted in terms of…
- Date of service (DOS)
- Type of Service
- Provider number
- Procedure code of CPT
- Place of service (POS)
- Billed amount

However, CO 18 isn’t the catch-all reason code for duplicates. If a duplicate Medicare claim gets submitted, it would receive the denial code OA 18.
Not confusing at all, right?
Well, to make matters worse it’s hard to consider CO 18 to be a true denial. Sometimes the payer has correctly identified that the claim is a duplicate of one already sent in. However, sometimes payers make mistakes with this denial code and incorrectly deny a corrected or altered claim.
How common is denial code CO 18?
The fact is that CO 18 is one of the most common types of denials.
Let’s put that statement to the test.
If you Googled the phrase “common denials in medical billing”, you would receive 253,000 results in 0.5 seconds.
The results feature several blog posts from different medical billing organizations that list the most common types of denials (thanks for the accuracy Google).
The top 5 results all list duplicate claim or service denials as one of the most common types.
Since the phrase that we searched wasn’t technical, neither were the answers provided by the organizations that landed on that page of results.
But as we’ve learned, CO 18 is the code associated with duplicate claim denials.
In other words, the statement at the beginning of this section is factual…even beyond this blog post itself.
Can I ignore denial code CO 18?
The short answer to the question of this section is, no. You simply cannot afford to ignore denial code CO 18.
Let’s walk through a real-world example featuring one of our clients.
One of our ~200-bed hospital clients received 928 CO 18 denials between 1/1/2022 - 6/30/2022. Based on our calculation, that’s ~$2.3 million worth of denials. However, that’s technically all loss revenue. Since this code deals with duplicate claim submissions, it’s likely that the majority of these claims were already submitted at one point and the insurance company is letting the hospital know.
In reality, maybe one-tenth of that number is actual money that the hospital needs to fight for.
In other words, some of those might not even be “true” duplicates, requiring staff reviewing and verification.
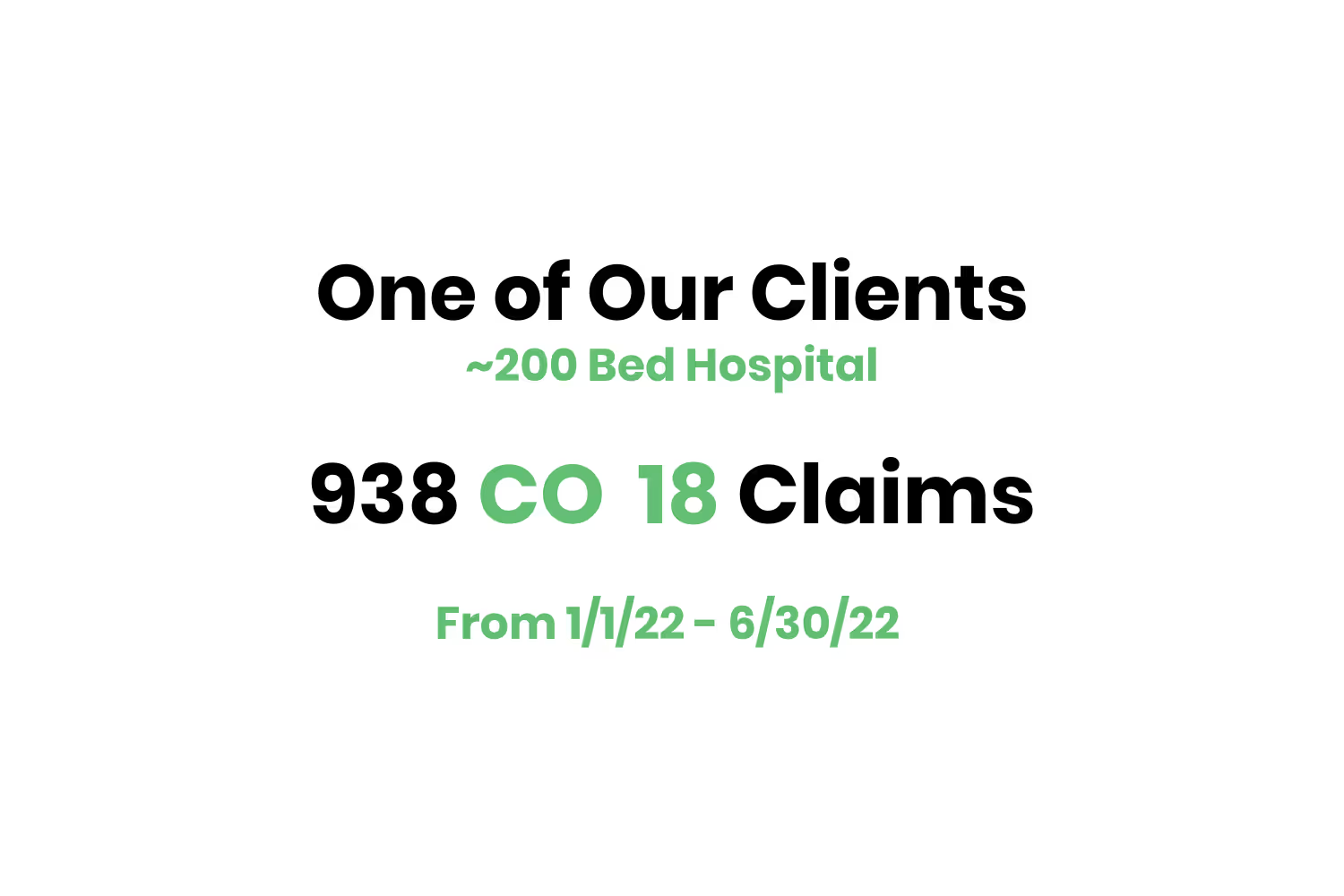
I didn’t throw in actual statistics from one of our clients to shame them. I wanted to show you actual data to give you a better idea as to how fast this type of denial stacks up.
As I alluded to a few sentences earlier, receiving this type of denial means one thing…reviewing and resubmitting them is another.
As an organization, you have to weigh the company resources involved with verifying and resubmitting every CO 18 denial received. Are they worth the extra effort? In most cases, the answer to that question is, “Yes.”
How do I avoid denial code CO 18?
In order to avoid denial code CO 18, you need to keep several things in mind depending on the type of claim you’re submitting.
If you’re sending a corrected claim, review payer guidelines to make sure you should be marking corrected claims with code 7 as the claim frequency code.
If you’re submitting a claim with multiple lines that could appear to be a duplicate, consider using modifier 59 after reviewing the payer's guidelines.
After all of this, though, you may be receiving 18’s because you sent a secondary claim to a payer, but the primary payer also sent the claim to the secondary payer. Seasoned medical billers call this kind of routing a "crossover."
You can tell if a primary payer is crossing claims over by looking at the CLP*02 of the electronic remittance advice (ERA). If this is a 19, it means that the payer processed the claim as primary, and crossed the claim over to the secondary. If they have done this, there is no reason to also send the claim!
If you believe that you’ve received a duplicate in error, you most likely will need to file an appeal with the payer.
Conclusion
After having a couple of decades under our belt in helping healthcare organizations make sense of their claim submission and denial management ecosystem, we’ve sensed a pattern.
There are certain denial codes that tend to come back to the organizations that submitted them more than others.
Out of all of them, though, CO 18 might be within the top 5 most common that our clients come across.
It rears its head more often than others because of mistakes that may occur on both sides…
- The submitter might’ve made a mistake in submitting the same claim more than once
- The payer might’ve made a mistake by denying a corrected claim
CO 18 is a code you need to not only pay close attention to from a workflow perspective but also because they require a lot of organizational resources to rework them.
Emphasize your product's unique features or benefits to differentiate it from competitors
In nec dictum adipiscing pharetra enim etiam scelerisque dolor purus ipsum egestas cursus vulputate arcu egestas ut eu sed mollis consectetur mattis pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus mauris aliquam ornare nisl purus at ipsum nulla accumsan consectetur vestibulum suspendisse aliquam condimentum scelerisque lacinia pellentesque vestibulum condimentum turpis ligula pharetra dictum sapien facilisis sapien at sagittis et cursus congue.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Incorporate statistics or specific numbers to highlight the effectiveness or popularity of your offering
Convallis pellentesque ullamcorper sapien sed tristique fermentum proin amet quam tincidunt feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.

Use time-sensitive language to encourage immediate action, such as "Limited Time Offer
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Address customer pain points directly by showing how your product solves their problems
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Vel etiam vel amet aenean eget in habitasse nunc duis tellus sem turpis risus aliquam ac volutpat tellus eu faucibus ullamcorper.
Tailor titles to your ideal customer segment using phrases like "Designed for Busy Professionals
Sed pretium id nibh id sit felis vitae volutpat volutpat adipiscing at sodales neque lectus mi phasellus commodo at elit suspendisse ornare faucibus lectus purus viverra in nec aliquet commodo et sed sed nisi tempor mi pellentesque arcu viverra pretium duis enim vulputate dignissim etiam ultrices vitae neque urna proin nibh diam turpis augue lacus.




