Everything You Need to Know About Denial Code CO 4
Here’s everything you need to know about denial code CO 4 including what it means, how to correct it and how to collect on it.

If you’re reading this you likely already know the giant, disheartening statistic that exists in medical billing…but I’ll tell you anyway.
According to AARP, 1 in every 7 submitted healthcare claims gets denied. If you didn’t know that statistic, I’m sorry.
Yes, it’s a discouraging statistic, but I can’t imagine it had that much of an effect on you because in order to be in medical billing you need to be resilient. After all, one of the biggest responsibilities that medical billers have is trying to make revenue off of claims that insurance companies don’t accept.

As a clearinghouse provider with over 20 years of experience, we help medical billers and healthcare organizations manage their entire claim ecosystem. Since we have so much history with insurance companies and the healthcare organizations that submit claims to them, we’ve noticed a pattern of common denials.
One such specific common denial code we see healthcare organizations struggle with is CO 4. Here’s everything you need to know about denial code CO 4 including what it means, how to correct it and how to collect on it.
What is denial code CO 4?
Denial code CO 4 is a Claim Adjustment Group Code (CARC).
The “CO” portion is an acronym for “Contractual Obligation”. Denials marked as “CO” mean that they’re based on the contract and as per the fee schedule amount.
Payers use this category of CARC codes when…
- A joint payer/payee agreement or regulatory requirement results in an adjustment that the member isn’t responsible for
- The provider’s charge exceeds the reasonable and customary amount and for which the patient is responsible
CO denials place financial responsibility on the provider. In other words, providers cannot assign financial responsibility to the patient or beneficiary.
There are over 200 different denial codes within the CO CARC category.
Just like with the statistic from earlier about the frequency of denials, any medical biller will tell you that you can’t overturn every denial. Sometimes, denials are a signifier of a workflow issue that happened before submitting the claim. For that type, you can’t just correct it and then resubmit them for payment. You have to use them as a learning experience and adjust your workflow accordingly for future submissions.
Luckily, CO 4 is not one of those types of denials…meaning that you can correct it and resubmit it.
But what is it?
Denial code CO 4 states that the code for the procedure…
- Isn’t consistent with the modifier used
- Or, that a necessary modifier is supposedly missing
What's a modifier?
Even though I just gave you what CO 4 means, it’s not overly helpful. It seems like the definition of the denial code is a code within itself that you need to crack.
To truly understand what this denial code is trying to tell us what happened to your claim, we need to define what a modifier is.
A modifier is a 2-character code consisting of letters or numbers that exist within CPT codes to indicate that a specific circumstance altered a performed service, but hasn’t changed in its definition or code.
Basically, modifiers provide additional information to help tell a story of a particular encounter.
Commonly used CPT modifiers are…
- 26: Professional component
- 59: Distinct procedural service
Should I care about denial code CO 4?
The truth about medical billing is that some organizations can’t keep up with how many denials they receive on a daily basis. Thus, they continue their daily operations and all of the denials they receive get added to the pile of yearly write-offs.
Advisory Board pulled massive headlines in 2017 when it published its Revenue Cycle Survey. The survey mentioned that hospitals had written off 90% more claims that year than six years prior due to an overwhelming amount of denials.
I know what you’re thinking, “That statistic is from 2017. There’s no way denial write-offs are still THAT common.”
Let’s fast forward a few years. In 2020, Change Healthcare reported that denials had risen 11% nationally. Based on what we learned from Advisory Board’s study in 2017, an increase in the denial rate leads to more write-offs.
But, CO 4 is just one denial code among thousands. Are you really missing out on that much revenue if you write it off?
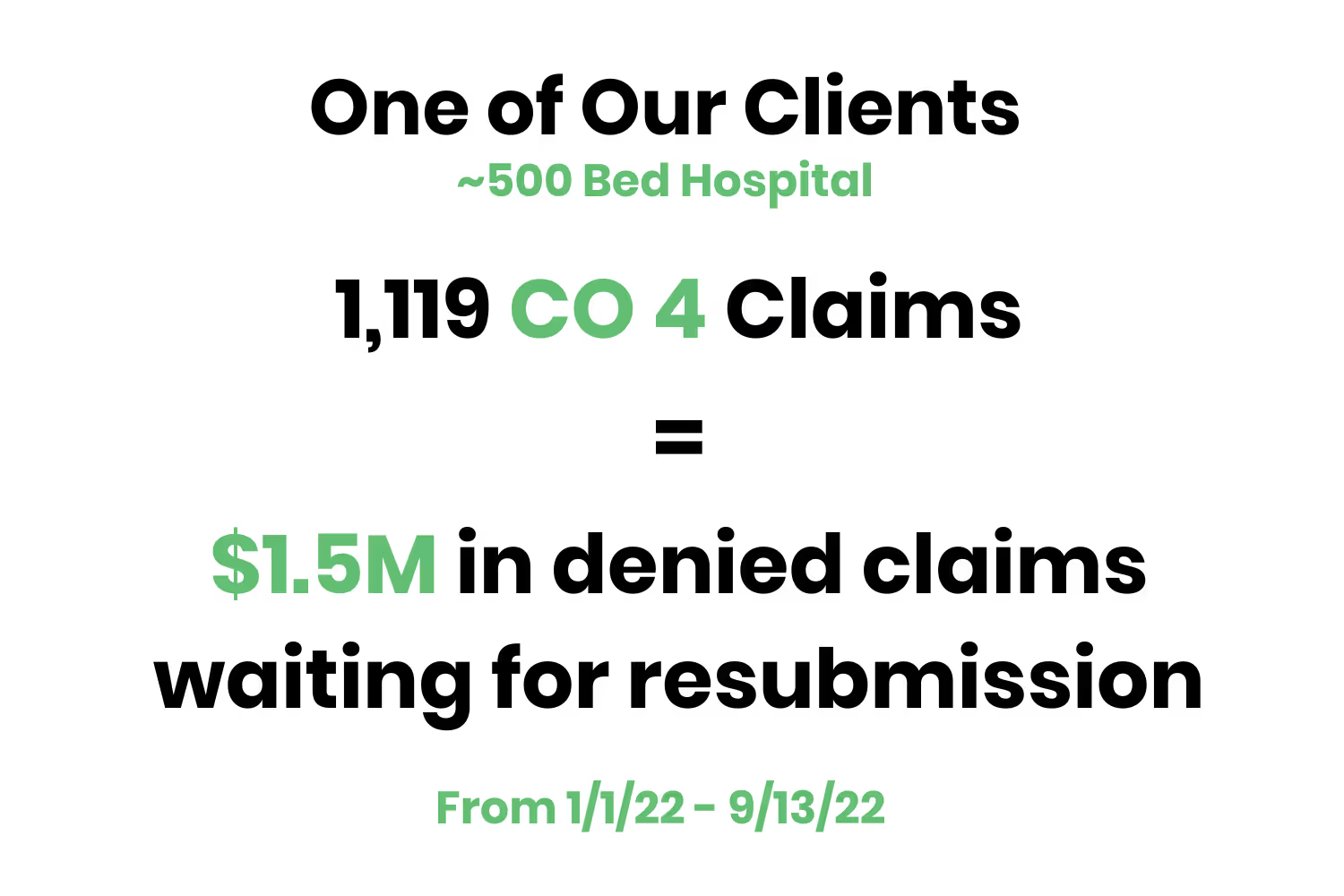
Yes! But, to further convince you, we took a look at our clearinghouse clients and ran some numbers. The results we found were astonishing.
More specifically, we took a look at the denial landscape for one of our ~500 hospital bed clients. From 1/01/22 - 9/13/22, that client had 1,119 claims that contained denial code CO 4. For better reference, that’s $1.5M in denied claims waiting for resubmission.
You see, CO 4 is one of the most common types of denials and you can see how it adds up. It also happens to be super easy to correct, resubmit and overturn.
In other words, if you’re running into CO 4 and you’re not resubmitting them…you’re leaving money on the table.
Through our research, we’ve found that though it would appear to be something simple to correct on a claim and rebill, either people are not doing that or are doing it and not being successful in getting the money!
How do I overturn denial code CO 4?
Alright, now that we’re on the same page regarding the monetary value that comes with correcting CO 4 denials and overturning them the next question becomes, “How do I overturn denial code CO 4?”
As I’ve alluded to throughout this post, overturning CO 4 denials isn’t overly difficult.
There are two options that you’re left with when you receive this denial code…
- Check if the modifier is consistent. If that’s not the case, get in touch with the coding team and ask them to recheck and assign the right code.
- Resubmit the claim
OR
- The claim submitted may have the appropriate modifier, but the insurance company denied it by mistake. If this happens, your next step is to reach out to the insurance’s claim department and send the claim back for reprocessing.
- If the insurance company disagrees regarding its mistake, appeal the claim with supporting documents.
How can a clearinghouse help?
Although reworking a denied claim that has the CO 4 status is easily resubmitted and overturned, it still requires effort.
Reworking CO 4 denials require additional company resources to correct a claim that was already worked and submitted previously.
In other words, healthcare organizations have to weigh the effort associated with resubmitting CO 4 denials in comparison to others to determine a priority list. After all, there’s a resubmission time limit on every denial that comes back.
The point I’m trying to make is that denial management is a tedious process…especially if it’s manual.
That’s one of the main reasons why your clearinghouse partner is such a valuable resource.
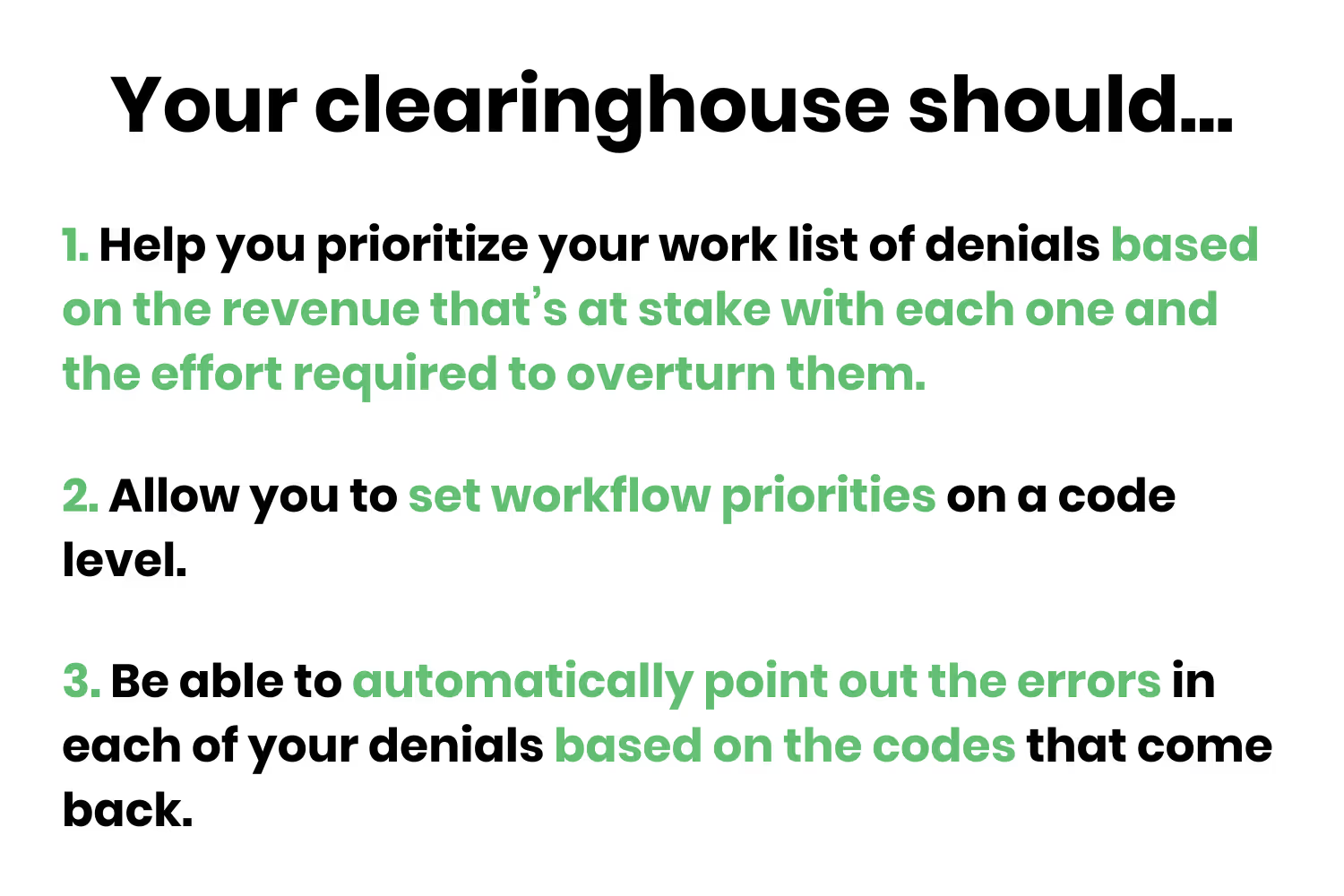
Your clearinghouse (like Etactics) should be able to help you prioritize your work list of denials based on the revenue that’s at stake with each one and the effort required to overturn them. Or, even better, allow you to set workflow priorities on a code level.
To make things even easier for you, it should be able to automatically point out the errors in each of your denials based on the codes that come back (our clearinghouse solution does this).
That way, when your staff sees CO 4 within your clearinghouse’s dashboard they’ll immediately know that it’s an easily overturned status and they can quickly correct and resubmit it.
Conclusion
Medical billing and coding aren’t easy. It’s a skill that requires a different level of resilience.
Dealing with denials alone is a tricky task because there are so many different codes and statuses that insurance organizations utilize.
Yet, not dealing with your denials at all and writing them off at the end of the year isn’t the solution.
Luckily, not every claim that comes back from insurance organizations unpaid requires a lot of company resources…denial code CO 4 falls under that designation.
Emphasize your product's unique features or benefits to differentiate it from competitors
In nec dictum adipiscing pharetra enim etiam scelerisque dolor purus ipsum egestas cursus vulputate arcu egestas ut eu sed mollis consectetur mattis pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus mauris aliquam ornare nisl purus at ipsum nulla accumsan consectetur vestibulum suspendisse aliquam condimentum scelerisque lacinia pellentesque vestibulum condimentum turpis ligula pharetra dictum sapien facilisis sapien at sagittis et cursus congue.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Incorporate statistics or specific numbers to highlight the effectiveness or popularity of your offering
Convallis pellentesque ullamcorper sapien sed tristique fermentum proin amet quam tincidunt feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.

Use time-sensitive language to encourage immediate action, such as "Limited Time Offer
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Address customer pain points directly by showing how your product solves their problems
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Vel etiam vel amet aenean eget in habitasse nunc duis tellus sem turpis risus aliquam ac volutpat tellus eu faucibus ullamcorper.
Tailor titles to your ideal customer segment using phrases like "Designed for Busy Professionals
Sed pretium id nibh id sit felis vitae volutpat volutpat adipiscing at sodales neque lectus mi phasellus commodo at elit suspendisse ornare faucibus lectus purus viverra in nec aliquet commodo et sed sed nisi tempor mi pellentesque arcu viverra pretium duis enim vulputate dignissim etiam ultrices vitae neque urna proin nibh diam turpis augue lacus.




