15 Ways to Deal with Difficult Patients
There are thousands of different reasons why a patient in your care is being difficult. But finding out why they’re acting out isn’t the most important aspect of these encounters. It’s how deal with them during this engagement that’s most important.

It doesn’t matter what your position is within the healthcare space. At some point or another, you’re going to have to deal with difficult patients. Unfortunately, that’s only one of the negative aspects with medical jobs.
There are thousands of different reasons why a patient in your care is being difficult.
They may be...
- Ridden with anxiety
- Frustrated with the care they’re receiving
- Angry with their diagnosis
- Defensive over their lifestyle
- Fearful about their family’s reaction
But finding out why they’re acting out isn’t the most important aspect of these encounters. It’s how you deal with them during this engagement that’s most important.
As a nurse, physician, or specialist, although every interaction is different from one another, it’s a career. What I mean by that is you’re doing a lot of the same things on a daily basis. While workload balance is a huge part of working within the medical space, that’s a different story.
The point I’m trying to make is that after a while your career desensitizes you. Fourth-year Stanford School of Medicine student, Natasha Abadilla, further emphasized this point in a blog post, “For medical trainees today, desensitization is almost inevitable.”
So what are the best ways to deal with difficult patients? What you do during these critical situations has a lasting impact on you and your clients.
Be Empathetic To Them
The best way to deal with any negative situation is through empathy. It’s the most human form of consoling.
First, if you work within a hospital or large healthcare facility, recognize your environment. You work at a place that most people don’t look forward to visiting.
While modern hospitals make a push towards a more welcoming atmosphere through interior design, yours may not be at that point quite yet.
Second, the patient might be acting out because of their newly learned long road to recovery. Breaking bad news is by no means an easy task but having to reconcile with it on a personal level is difficult too.
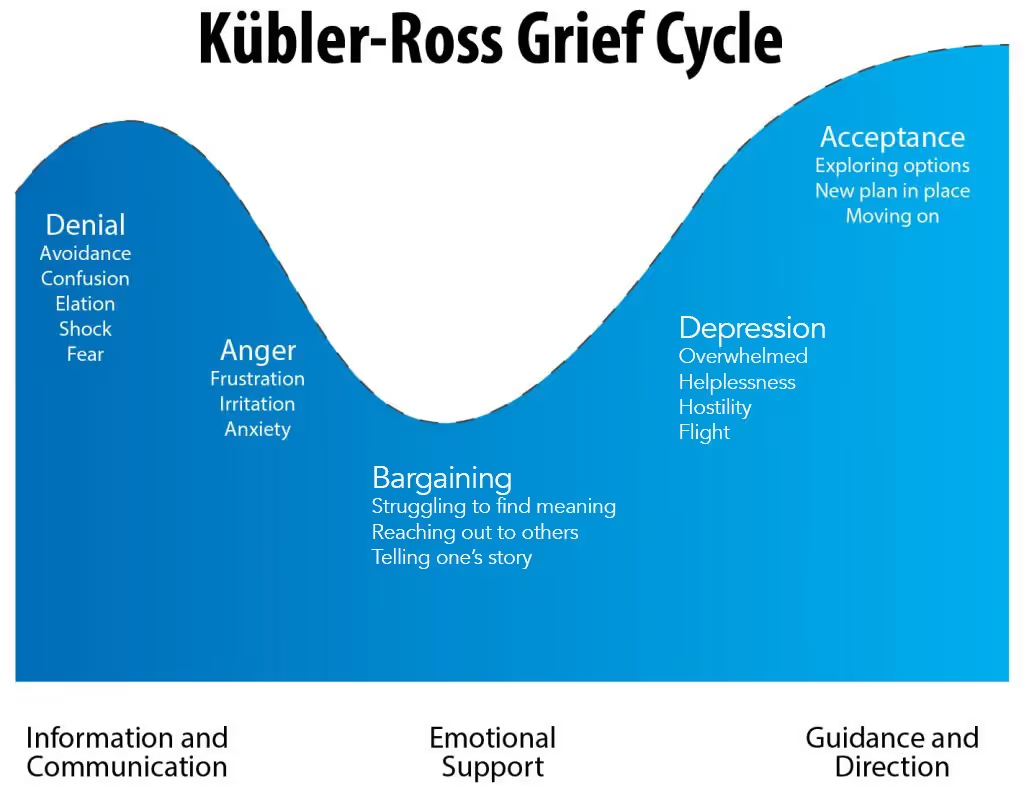
Depending on the severity of their diagnosis, they may go through a form of Elisabeth Kübler-Ross’ stages of grief; denial, anger, bargaining, depression, acceptance.
In situations when you’re forced to deal with difficult patients, the best thing you can do is to show that you care about them.
Listen - Let Them Tell Their Story
Outside of showing empathy, listening is the next most important way to deal with difficult patients. You can’t do one without the other. But it’s also because it allows your client to let off steam.
Disclosing stress is a coping method, that’s a proven fact. It also happens to be a two-way street. In order for it to happen there needs to be someone venting and another person listening.
If the patient needs to get something off their chest, let them and be attentive. It helps establish a bond with that patient while making caring for them easier. In fact, patients are 13% more willing to collaborate with their care plan if they’re recognized.
Body Language Speaks Volumes
Of course, while they’re yelling, venting or frustrated there’s more to it than listening. Your body language will tell the true story of your emotions and how you’re feeling over your verbal reassurances.
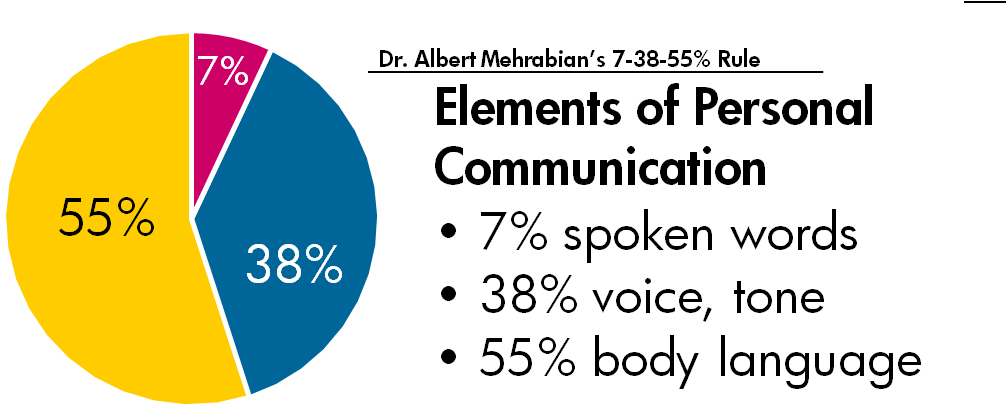
One of the most common myths we hear about body language is that it’s 93% of communication. This comes from a study conducted by Dr. Albert Mehabrian and it’s often misquoted. Communicating non-verbally doesn’t deliver 93% of your entire message. Instead, it reveals underlying emotions, motives and feelings in an instant.
The best way to stay aware of your body language is by keeping a cool head. Pay attention to what you’re doing with your facial expressions.
As your patient vents or tells you their frustrations, maintain eye contact with them. What’s important here is that you don’t stare them down. That could come off as threatening and escalate the situation.
A good rule of thumb to control your body language is by recognizing the signs of a difficult client situation. This comes with experience but once you know them you can get in the right mindset and mediate the situation.
Acknowledge The Elephant in The Room
You’ve been in a social situation where there’s underlying tension at some point in your life. It’s not enjoyable but this same circumstances will also present themselves in healthcare.
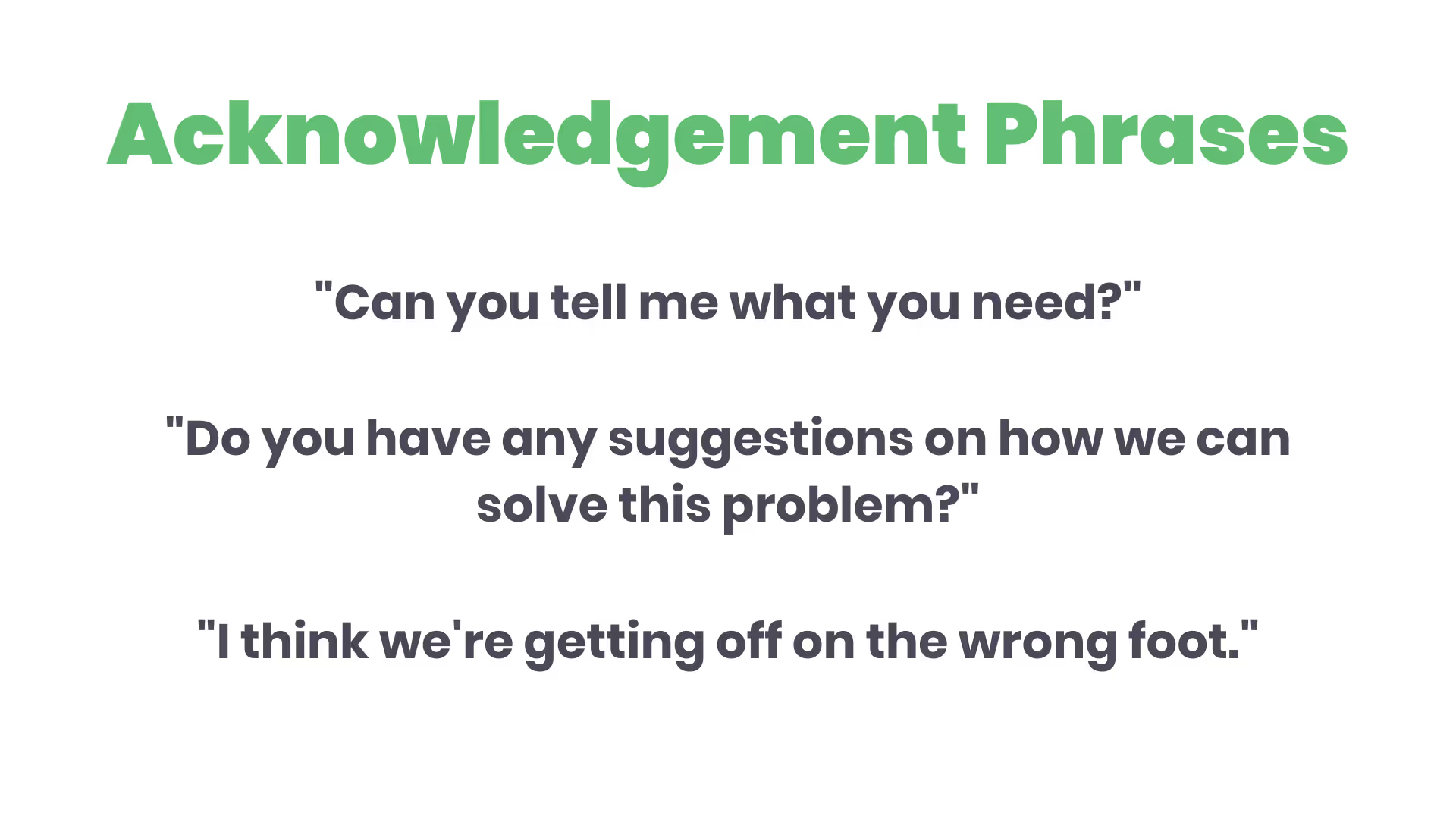
When this happens, it’s your professional responsibility to acknowledge the tension. When doing so, ask something along the lines of “I think we’re getting off on the wrong foot.”
You can also ask the patient for their ideas by saying, “Do you have any suggestions on how we can solve this problem?”
Once you do this, they’ll be much more willing to open up about a conflict. Which allows you to continue the visit productively.
Stay Calm and Keep Composure
You’re a professional within the healthcare space, which is incredible. This also means that when something bad happens a patient will look to you for advice. This is most likely one of the reasons why you went into the medical field in the first place.
But it also means that when something bad happens to a patient, they might lash out. If they do, it’s also your responsibility to recognize that they’re most likely not upset at you directly. Instead, they’re riddled with anxiety. Their current mental state has led them to act out.
Thus you must maintain your composure, you’re the expert that the patient goes to for answers. If they have questions, make sure to answer them to the best of your abilities.
Remaining calm will help you defuse the situation.
Know Where Your Strengths Lie
This isn’t the first time you’ve been tough social position. In the past, what was your most effective strategy to diffuse a hostile situation? Play to your strengths.
If you shine most with your sense of humor, use it to try and improve the patient’s mood.
Maybe you like a more gracious approach. Staying accommodating no matter how they’re acting may change their entire demeanor.
You may get easily discouraged by negative comments from difficult patients. If so, take some extra time for yourself to regroup so you can move on from the situation more effectively.
Set Clear Boundaries
Patients who stay at hospitals need attention, there’s no denying that. But sometimes they’ll ask for more attention than what’s warranted. Giving in to their requests is a slippery slope. If you do so for one, you’ll soon find that you have no time for others in need.
To avoid this from happening to you, set yourself time limit boundaries. It could be an increment you want within reason but test it out as you go. As you get more used to telling a demanding patient that you’ll see them again within 15 or 30 minutes you’ll find that days are less stressful.
If the patient is newly admitted, they may get frustrated or angry with you at first when you don’t give in to their request. However, over time they’ll get used to it and be able to empathize with your busy schedule.
Abuse is Unacceptable
Regardless of the conflict, any form of abuse isn’t acceptable. It’s not in your job description to be the victim of abuse.
Every provider has a different definition of what they determine as verbal abuse. As you provide care to patients your line will form.
If a patient crosses that line, you can’t get in the habit of accepting abusive behavior. Tell them firmly that their behavior is unacceptable. If they continue to act out, don’t hesitate to alert your supervisor.
If you’re ever in a situation when you feel physically threatened or uncomfortable, call security.
Stay Engaged in The Conversation
Most of the time, difficult patients just want acknowledgment. They want your attention in some form.
After you’ve listened to their frustrations, maintained appropriate body language, and established clear boundaries you’re still not done with this uncomfortable situation. At this point, the last thing you’ll want to do is escalate things further.
But to keep things cordial, you have to engage in the conversation. If you don't, the patient will think that you’re ignoring them.
Throughout the situation, use their first name. That way they know you’re listening and engaged. Also, speak in a confident tone, even if the patient is yelling. Third, articulate how you respond. Methodically choosing your words will keep you focused on what’s happening.
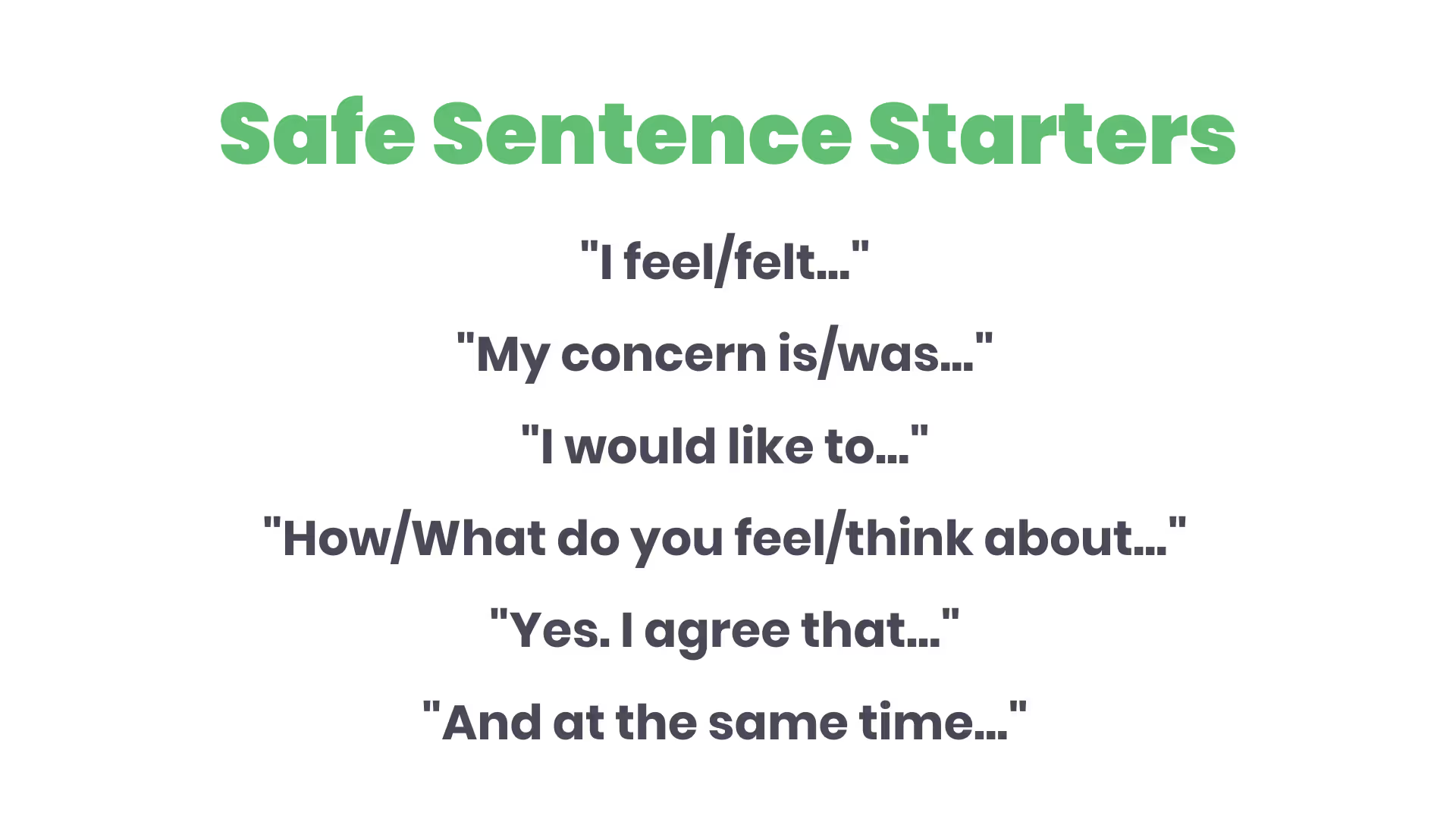
Psychology Today has a list of 6 safe sentence starters to use when having sensitive discussions. These phrases will help you glide through this conversation gracefully while conveying that you want to proceed in a collaborative manner.
Stay Professional No Matter What
The doctor-to-patient relationship is both personal and intimate. The majority of patients recognize that there are boundaries to maintain in this type of relationship but that’s not always the case.
Difficult patients aren’t always the ones who lash out. Sometimes they may become clingy. What started out as a thankful client who never shied away from complimenting your abilities might turn into a nightmare.
They may make demands that most wouldn’t, putting your career in the balance. Or they could become needy and ask to spend more time with you, giving you less time to unwind after stressful days.
This type of patient is particularly hard to navigate. Do so poorly and them leaving your practice is the least of your problems. They could go on to spread their negative opinions to their network of family, friends, and coworkers, diminishing your word-of-mouth marketing strategy.
But by staying professional throughout the entire medical relationship, you’ll avoid this situation from happening altogether. This doesn’t mean you can’t be personal while at work. Instead, it helps diminish relationship grey areas.
Set Terms Within Policies
As you know, almost everything within this industry requires strict policies, even for those who ditch their appointments. Certain treatments or diagnoses require a patient to sign a contract. This contact gives guidance on treatment to include medication dosage and when to take it.
To legally protect yourself and your clients, ensure that comprehensive, written policies back your contracts.
Each policy should state clearly what’s expected in a professional relationship between a patient and a provider.
When All Else Fails - Refer to Outside Help
If you’ve exhausted all of your ways to remedy the situation and the client is still dissatisfied or upset, you can suggest outside help to them. This is the last helpful resource you can use when dealing with difficult patients but it might be necessary under certain circumstances.
If you go this route, understand that this is an extremely sensitive topic. Introducing this idea into the discussion may add fuel to the fire if not approached correctly. They may feel as though you’re abandoning them or can’t help them anymore.
But it’s important to remember that you can’t be a heal-all for everyone you see. Some may need and receive a lot of benefits from speaking with a mental health professional, social worker, or chaplain.
Termination as a Final Option
If you’ve recommended outside, professional help to the patient and they’re still acting out you’re left with one final option. Termination doesn’t happen often but maybe the only choice you’re left with.
If this happens, write the client a concise termination letter. Ensure that it states they violated the physician-patient relationship.
First, identify the last visit date. Second, you’ll have to provide the patient with adequate access to prescription medication post-termination to ensure continuity of care.
Third, notify that you’re sending a copy of their chart and information to they’re a new provider.
Fourth, if you’re sending this letter through the mail, ensure you’re sending it through first-class and registered mail via the USPS due to its sensitivity.
Finally, understand that you don’t need to be overly detailed within this letter, keep it short and professional.
Once It's Over, It's Over
After dealing with a difficult patient, don’t let it ruin your day by dwelling on every little detail of what happened. Instead, take a few moments for yourself.
Most likely, you’re saying to yourself, “I don’t have time to take to myself, there’s a lot of other patients that need me.”
But recouping is essential. Take a deep breath to regather your senses. If you need more than a deep breath, look towards meditation. Not only can it destress you, but it can also make you up to 120% more productive.
When you’re ready, get back out there.
Keep Yourself Grounded Off The Clock
In every industry, our careers can get stressful. Although there will always be both good and bad days, the last thing you want to do is bottle up stress.
Self-care is an essential part of keeping a cool head. It’s a great way to diminish sleep deprivation, pain, and stress.
There are thousands of activities you could do to stay grounded outside of work hours including…
- Hiking
- Running
- Yoga
- Biking
- Mediation
Participate in whichever activity you resonate with the most. Over time you’ll notice that your ability to handle situations with difficult patients gets easier.
Conclusion
There’s no way to avoid the eventual interaction with difficult patients, it’s bound to happen at some point along with your medical career.
As a healthcare professional, people will come to you with all different types of ailments, mood disorders, fears, and a plethora of other complications. They’ll come from diverse backgrounds with lifestyles you may not always agree with.
But outside of caring for them individually, all that is noise. Objectivity, honesty, empathy, and your undivided attention is the road to giving each of your patients the best care.
Emphasize your product's unique features or benefits to differentiate it from competitors
In nec dictum adipiscing pharetra enim etiam scelerisque dolor purus ipsum egestas cursus vulputate arcu egestas ut eu sed mollis consectetur mattis pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus mauris aliquam ornare nisl purus at ipsum nulla accumsan consectetur vestibulum suspendisse aliquam condimentum scelerisque lacinia pellentesque vestibulum condimentum turpis ligula pharetra dictum sapien facilisis sapien at sagittis et cursus congue.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Incorporate statistics or specific numbers to highlight the effectiveness or popularity of your offering
Convallis pellentesque ullamcorper sapien sed tristique fermentum proin amet quam tincidunt feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.

Use time-sensitive language to encourage immediate action, such as "Limited Time Offer
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Address customer pain points directly by showing how your product solves their problems
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Vel etiam vel amet aenean eget in habitasse nunc duis tellus sem turpis risus aliquam ac volutpat tellus eu faucibus ullamcorper.
Tailor titles to your ideal customer segment using phrases like "Designed for Busy Professionals
Sed pretium id nibh id sit felis vitae volutpat volutpat adipiscing at sodales neque lectus mi phasellus commodo at elit suspendisse ornare faucibus lectus purus viverra in nec aliquet commodo et sed sed nisi tempor mi pellentesque arcu viverra pretium duis enim vulputate dignissim etiam ultrices vitae neque urna proin nibh diam turpis augue lacus.


.avif)

