[ANSWERED] What is the Revenue Cycle in Healthcare?
You can’t have a solid revenue cycle management process in place if you don’t know what it is. Let’s explain what the revenue cycle in healthcare is.

Over 33% of hospitals are operating on negative margins according to a study by the American Hospital Association. Health systems have faced large financial losses within the past few years. Effecting the overall financial stability of organizations both large and small.
This, of course, is partially due to the covid pandemic. With the public health crisis rocking healthcare foundations around the world, staff shortages, rising expenses, and supply chain problems still cause issues even to this day.
When you think of hospitals or doctor’s offices, you think of their job making sure to prioritize patient care. While this is true, we can sometimes forget healthcare facilities operate as businesses. Not only do healthcare workers need to focus on the patient experience, but also ensure sustainability as a business.
While patient's focus on getting healthy, healthcare facilities need to also make sure the business stays stable.

Revenue cycle management (RCM) makes sure hospitals and other healthcare organizations can stay open. Like any other business, healthcare facilities can close due to a lack of revenue.
Between January 2013 and February 2020 over 100 rural hospitals had to close due to financial troubles.
But…you can’t have a solid revenue cycle management process in place if you don’t know what it is. Let’s explain what the revenue cycle in healthcare is.
What is Revenue Cycle Management (RCM)
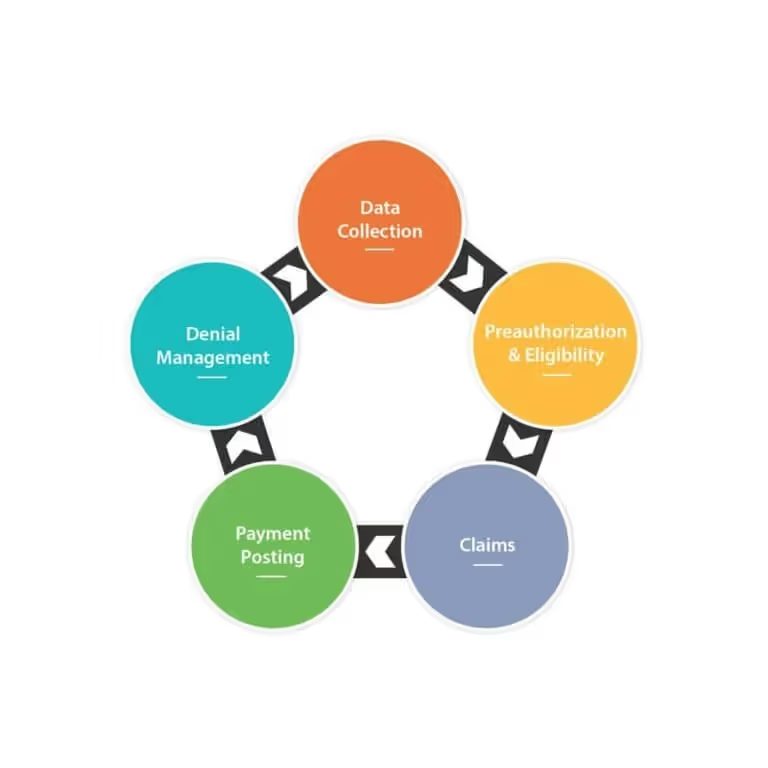
So all this “revenue management” stuff sounds great (I know I’m revved up), but I should explain what it is. Healthcare revenue cycle management is the process that tracks revenue from patient engagements. This includes everything from their initial visit with the healthcare system to the final payment of their balance.
The RCM process assists with the administrative functions that handle the capture, management and collection of patient payments.
The average American spends roughly $12,530 in deductibles and premiums each year, not including the out of pocket expenses. Keeping track of all this cash flow needs a trustworthy and secure system to file data and keep balances accurate.
Let’s take a moment and go over the stages of the healthcare revenue cycle.
Registration
First, healthcare providers need to collect patient information for verification before their appointment.
More specifically, I’m talking about insurance coverage. This pre-registration information follows after a patient schedules an appointment to seek medical services.
Once the patient arrives they’ll need to register more information to establish their medical record.
By having all the correct information upfront, it’s easier to get medical billing correct the first time. Insurance verification allows for smoother billing and coding practices.
Registration provides a solid foundation for optimal revenue cycle management. When the administration takes time to get the correct information it makes it easier and faster to collect patient payments.
Medical Coding
Once the visit is over, the provider must submit the patient’s claim. To do this, medical coders refer to the ICD-10 or CPT code that corresponds with the treatment given. This, in turn, determines how much reimbursement the entity will receive from the patient’s insurance plan.
Making sure to select the appropriate code is an important key in this stage of the cycle. Errors in front-end tasks like this remain one of the top reasons for claim delays and/or denials. Proper denial management using RCM systems makes claim submission more accurate.
Imagine you make an appointment to visit your doctor for a routine check-up. This visit includes bloodwork and a physical exam. But the code sent to the payer is incorrect. This would be a reason for a claim denial, along with other factors such as incorrect registration information or out-of-network services. Trust me, the last thing you want is to receive a denied claim with denial code CO 18.

Almost 1 in 5 insurers report they deny more than 30% of in-network claims. Without the help of proper revenue cycle management, it might take weeks for a provider to hear back about a claim denial. Naturally, delays in receiving that reimbursement for the services.
Billing/Collections
Once the service coding is correct, the practice sends the claim to private or government payers for reimbursement.
As long as the claim processes, back-end office duties can begin.
These tasks include…
- Payment posting
- Statement processing
- Payment collections
- Handling any claim denials
Anything that the payer doesn’t cover is then sent to patients. From there, it’s up to the patients to pay their existing balance with the provider. Healthcare revenue cycle management helps keep entities organized with their patient information and receive payments promptly. But, there are both internal and external factors that can still affect the collection of patient revenue.
The Challenges of Healthcare Revenue Cycle Management
Bills and claims usually go through processing over long periods. Claims can go back and forth between payers and providers for weeks. This depends on whether information taken during registration is accurate, whether the codes match services and procedures, and other factors.
It can even take months to resolve certain billing issues. If you receive a claim denial, it can be a few days until the provider has this information, which in turn pushes off payment even more.
Patients not being able to pay their bills is another reason for a delay in the revenue cycle. People don’t always have the means to pay their full balance, especially those who have chronic illnesses and are habitually at the doctor’s.
Both of these challenges fall under the umbrella of external factors and can be either difficult or impossible to control.
Payment Collection
If you’re in the healthcare field, you aren’t a stranger to the challenges associated with collecting patient payments. Ideally, we’d love to know the secret behind collecting payments at the time of service.
But I’ve got to be realistic with you. Nearly 23 million Americans owe medical debt. For those who don’t want to do the math, that amounts to 1 in 10 adults!

Many patients are unable to pay medical bills upfront. This can be due to high deductibles and/or financial issues. A study from 2020 revealed that patient collection of $1,000 and over takes more than a month for 78% of healthcare providers. So it’s up to these providers to find a balance between collecting these payments within a timely manner and avoiding driving patients away.
Coding Issues
Coding is one of the challenges you can have more control over, but there are still problems that will arise you can’t plan for.
Coding errors by staff members could lead to delayed or denied claims, slowing your reimbursement. Sloppy documentation by physicians or other healthcare professionals could also be a factor in a code error.
Best Practices For Revenue Cycle Management
Now that we’ve gone over the basics of the revenue cycle, I’m sure you’re eager to get cracking.
One way to go about having a reliable and orderly system is by outsourcing their revenue cycle management.
This strategy serves to better manage patients’ bills and process claims. In turn, allowing for quick and easy access to records whenever you may need them. No more digging through your computer to find a PDF you accidentally forgot to rename.
RCM software (we provide this) can help providers and their teams streamline front-end tasks and even help automate the more mundane day-to-day duties.
This includes informing patients of appointments, billing reminders, and providing quick and easy payment options through an online portal.
Outsourcing claims to a clearinghouse (we provide this too) also reduces the amount of time between submission and receiving payment. A clearinghouse is an electronic platform that’s an important tool to have in your RCM toolbelt.
Sending your claims through a clearinghouse before submitting them to the insurance carrier cuts down on denied claims. The industry calls this feature that clearinghouses provide “claim scrubbing” and it’s worth it.
Claim scrubbing prompts your team to enter all the correct information and notify you immediately if there is a mistake in a claim. Instead of waiting a week to hear back from the payer, clearinghouses let you know immediately if any errors exist within your patients’ claims.
Optimize Your Claim Management Process
The fact is that healthcare professionals need to always be aware of their revenue cycle status. After all, it’s hard to provide the best care to patients without collecting revenue.
Meanwhile, the healthcare industry continues to change and evolve along with technology. Keeping pace with changes while adjusting your management system can help you stay competitive.
Revenue cycle management comes down to this: being able to integrate traditional tasks with digital intake for better patient access.
Emphasize your product's unique features or benefits to differentiate it from competitors
In nec dictum adipiscing pharetra enim etiam scelerisque dolor purus ipsum egestas cursus vulputate arcu egestas ut eu sed mollis consectetur mattis pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus mauris aliquam ornare nisl purus at ipsum nulla accumsan consectetur vestibulum suspendisse aliquam condimentum scelerisque lacinia pellentesque vestibulum condimentum turpis ligula pharetra dictum sapien facilisis sapien at sagittis et cursus congue.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Incorporate statistics or specific numbers to highlight the effectiveness or popularity of your offering
Convallis pellentesque ullamcorper sapien sed tristique fermentum proin amet quam tincidunt feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.

Use time-sensitive language to encourage immediate action, such as "Limited Time Offer
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Address customer pain points directly by showing how your product solves their problems
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Vel etiam vel amet aenean eget in habitasse nunc duis tellus sem turpis risus aliquam ac volutpat tellus eu faucibus ullamcorper.
Tailor titles to your ideal customer segment using phrases like "Designed for Busy Professionals
Sed pretium id nibh id sit felis vitae volutpat volutpat adipiscing at sodales neque lectus mi phasellus commodo at elit suspendisse ornare faucibus lectus purus viverra in nec aliquet commodo et sed sed nisi tempor mi pellentesque arcu viverra pretium duis enim vulputate dignissim etiam ultrices vitae neque urna proin nibh diam turpis augue lacus.




