The Adjudication of Claims: An Ultimate Guide
Although the adjudication process of claims isn’t something that your organization has complete control over, there are workflows you can put in place right now to better ensure that better your chances of getting paid. Here is our ultimate guide to the adjudication of claims.

You submit a patient’s claim to their insurance payer, their payer takes a look at it and they pay you. Easy enough, right?
Although that statement is technically true regarding the claim submission process, it’s definitely not easy. Every experienced medical biller will tell you that there is a lot more involved in the three steps I just listed and that it’s the minutiae that matter most within each step.
After all, there’s a reason why 30% of insurance claims get denied on their first submission.
Regardless of how one particular claim gets denied, all of them go through the same overarching process once received by a payer… adjudication.
Although the adjudication process of claims isn’t something that your organization has complete control over, there are workflows you can put in place right now to better ensure that better your chances of getting paid.
Here is our ultimate guide to the adjudication of claims.
What is Claim Adjudication
In a nutshell, claim adjudication is the process that every insurance payer goes through to determine how much they owe a provider based on a claim that they received.
While working through this process, the insurance payer makes one of three decisions per claim…
- To pay the claim in full
- Reduce the amount paid to the healthcare organization
- Deny the claim
The ideal scenario for the healthcare organization that submitted the claim is that the payer decides to pay in full. When that happens, the healthcare organization will see a credit appear in its bank account for the full amount.
In some cases, a payer will decide that they’ll only pay a portion of what they owe according to the claim back to the healthcare organization. This scenario happens when the payer finds that the billed service level isn’t appropriate according to the diagnosis or procedure codes. When this happens it’s a disappointing situation, but at least there is SOME form of compensation.
By far, the worst scenario that can come as a result of claim adjudication is a denial. Denials happen when there are blatant errors in a submission. When a denial occurs, the payer sends the claim back to the healthcare organization that submitted it along with a reason for the denial. Unfortunately, payers don’t provide compensation for denials until they’re fixed and resubmitted (more on that later).
This is all helpful information, but what does the adjudication of claims process actually look like?
Claim Adjudication Process Flowchart
Just like with the Electronic Data Interchange (EDI) enrollment process, claim adjudication looks different for every payer.
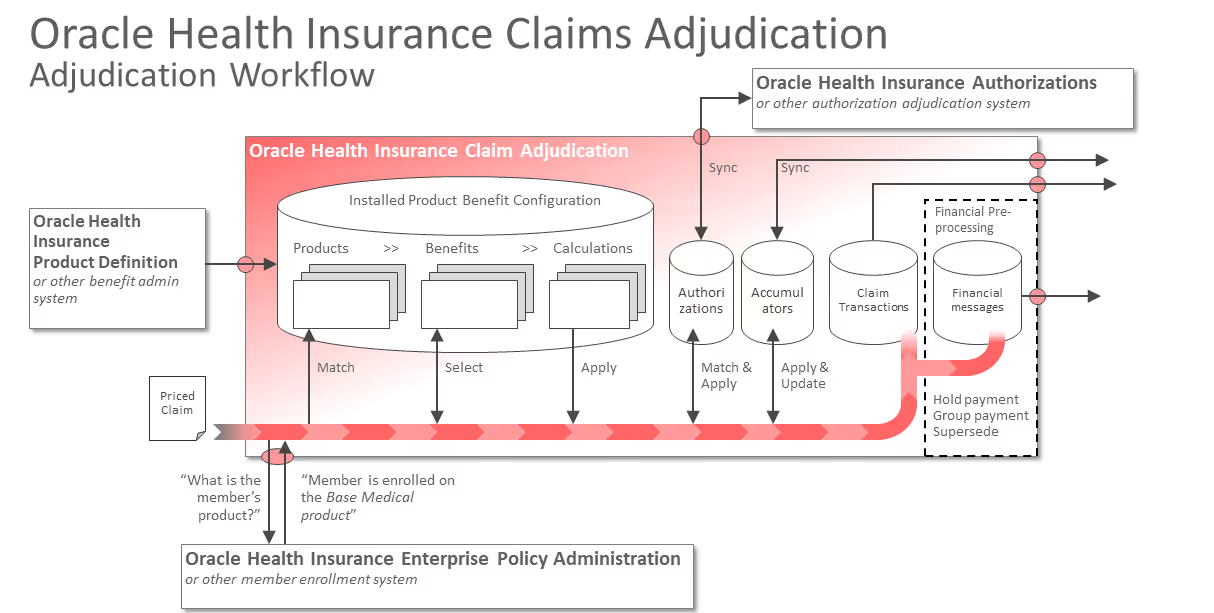
The flowchart above comes from Oracle Health Insurance. This payer has an entire webpage that’s devoted to explaining its adjudication workflow.
As you can tell from the flowchart, the process is pretty straightforward, right? I’m being facetious. It’s great that Oracle Health Insurance took the time to create a flowchart that graphically explains its process for claim adjudication, but it’s definitely not easy to understand.
Basically, the takeaway from this payer’s flowchart is that you submit the claim and it runs a series of checks and balances against it based on the associated plan.
It’s a neat-looking graphic, but it’s not super helpful. Let’s break down the steps that most payers take during adjudication.
Step 1: Initial Processing Review
The first step in the adjudication process is the initial processing review. Believe it or not, this is where many claims end up getting denied.
During this first step, the payer checks the claim for simple errors or omissions. More specifically, payers look at the accuracy of…
- The patient’s name
- The patient’s subscriber identification number
- The service code
- The date of service
- The diagnosis code
- The patient’s gender
If a claim fails this step, it will get sent back to the organization that submitted it. Of course, that means it receives a “denied” status. Denials aren’t the end of the world because you can resubmit them…but reworking and resubmitting them costs company resources.
Step 2: Automated Review
If a claim passes the first initial review step, it moves into the automated review.
The automated review step takes a more detailed look as to whether or not the claim matches up with the payer’s policies. More specifically, this step looks for whether or not…
- The patient was eligible on the date of service.
- Pre-certification or authorization is not present and/or not valid.
- The claim submitted is a duplicate.
- The timely filing deadline has passed.
- The diagnosis or procedure code is invalid.
- The services performed weren’t medically necessary.

Step 3: The Manual Review
The third step is when a trained, professional medical claim examiner steps into the spotlight. In some cases, the examiner might also bring in a nurse or physician to take a look at the claim as well.
Anyway, most payers tend to agree that this is a necessary guardrail in the process. It isn’t out of the ordinary for a medical record request to take place during this step. Requests of that nature won’t happen every time, usually only for unlisted procedures to determine medical necessity.
Step 4: Payment Determination
The last two steps within the standardized adjudication process happen only after a claim passes the three phases of review. In other words, it’s how healthcare organizations receive payment from payers.
From a high level, there are only three key types of payment determinations that claim experience…
- Paid - The payer determined that the claim it received is reimbursable
- Reduced - The payer determined that the service level billed for the diagnosis is too high, thus it “downcoded” the procedure code to a lower level according to the claim examiner.
- Denied - The payer determined that the claim it received is not reimbursable

Step 5: Payment
I have to confess something to you before we continue…in the adjudication process, receiving money from a payer isn’t called “payment”. The payment as the result of the adjudication of claims is either called remittance advice or explanation of payment.
Why isn’t it just called payment?
Payers don’t provide just money. Alongside the money or credit associated with the claim also comes explanations. These explanations provide detail regarding the reasons for…
- Payment
- Reduction of payment
- Adjustments
- Denial and/or uncovered charges
Of course, that’s my more easily understood explanation. More specifically, these reasons exist as the following key data points…
- Payer Paid Amount
- Approved Amount
- Allowed Amount
- Patient Responsibility Amount
- Covered Amount
- Discount Amount
- Adjudication Date
Appealing Claim Denials
Out of all the payment determination statuses that a claim could receive during a payer’s adjudication process, “denied” is the most frustrating to deal with.
Do you remember during the introduction of this blog post when I stated that 30% of all claims get denied? I wouldn’t have put that statistic in the introduction if it wasn’t one of the biggest pain points that healthcare organizations deal with when it comes to dealing with payers.
You see, when a claim doesn’t pass all of the checks during a payer’s adjudication process, it gets sent back to the organization that originally submitted it with a “denied” status.
To put it bluntly, a denied claim means that the insurance payer isn’t paying you for the services you provided to a patient.
The immediate reaction to the statement above usually involves a few expletive statements targeted toward payers.
Yet, a denial doesn’t mean the end of the world.
Payers allow for the resubmission of denied claims. This process is what’s referred to as appealing.
Healthcare organizations establish internal claim appeal processes that usually include the following steps…
- Locating the errors in the claim
- Fixing the errors
- Filling out the payer’s appeal letter
- Resubmitting the denied claim
Outside of not receiving payment from the payer, denials also require organizational resources to rework and resubmit the claim as an appeal. Thus, getting an appeal accepted ends up costing the organization more than the original submission.
In some cases, healthcare organizations often evaluate whether or not appealing denials is even worth it.
The clear argument against that is the adage, “money is money”. But the better answer is that establishing precise workflows for claim submission AND appealing lowers all operating costs.
Adjudication Made Easier with a Clearinghouse
Clearinghouses make adjudication less stressful.
If you take anything away from this blog post, that’s what you should keep in mind.
At their core, clearinghouses take the burden off healthcare organizations’ shoulders by baking in pre-emptive checks on all claims before submission.
Here’s how.
Perk 1: Payer Connections
Clearinghouses act as a one-stop shop for every type of healthcare organization.
I’ve alluded to this already, but every payer has different EDI enrollment AND adjudication requirements. On top of all of that, the majority of patients that healthcare organizations see are all going to use different insurance payers.
Clearinghouses already have established connections with thousands of payers (we have these). In other words, signing up with the right clearinghouse instantly takes those tedious tasks off the healthcare organization’s plate.
Perk 2: Claim Scrubbing
Since clearinghouses natively know what the adjudication process requirements for thousands of payers look like since they’re connected with them, part of their value-add is claim scrubbing.
Claim scrubbing is the process of submitting a claim to the clearinghouse BEFORE the payer. When this happens, the clearinghouse compares the claim to the payer’s requirements and provides feedback on it.
Claim scrubbing exists as a “spell check” functionality. The clearinghouse points out any errors prior to payer adjudication so that the healthcare organization doesn’t experience a denial.
Perk 3: Predicting with Claim Status
Obviously, there are a lot of processes happening during claim adjudication that are outside of the control of the submitting healthcare organization.
The only form of “control” that the healthcare organization has after they’ve submitted a claim to a payer is by making sure it was 100% accurate BEFORE submission occurred.
However, some clearinghouses (like ours) provide the ability for healthcare organizations to gain insight into the status of their claim submission.
Finding out the status of a claim makes it easier for the healthcare organization to predict its revenue sooner. If the organization checks the status of its submitted claim and it’s not looking good, it can also preemptively kick off its appeal process.
Think Dominos Tracker, but receiving money is at the end of it instead of pizza.
Conclusion
Of course, nothing is as easy as it sounds when it comes to working with insurance payers. The adjudication of the claims process is no different.
Adjudication is the industry phrase that’s used to describe the internal process that payers go through to determine whether or not they’re reimbursing the organization that submitted it.
It’s definitely up there in terms of being one of the most painstaking revenue cycle processes…especially since a lot of it is out of the submitting organization’s control.
Yet, partnering with a clearinghouse (like Etactics) makes adjudication easier to swallow by streamlining front-end processes and providing insight into each submitted claim’s status.
Emphasize your product's unique features or benefits to differentiate it from competitors
In nec dictum adipiscing pharetra enim etiam scelerisque dolor purus ipsum egestas cursus vulputate arcu egestas ut eu sed mollis consectetur mattis pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus mauris aliquam ornare nisl purus at ipsum nulla accumsan consectetur vestibulum suspendisse aliquam condimentum scelerisque lacinia pellentesque vestibulum condimentum turpis ligula pharetra dictum sapien facilisis sapien at sagittis et cursus congue.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Incorporate statistics or specific numbers to highlight the effectiveness or popularity of your offering
Convallis pellentesque ullamcorper sapien sed tristique fermentum proin amet quam tincidunt feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.

Use time-sensitive language to encourage immediate action, such as "Limited Time Offer
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Address customer pain points directly by showing how your product solves their problems
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Vel etiam vel amet aenean eget in habitasse nunc duis tellus sem turpis risus aliquam ac volutpat tellus eu faucibus ullamcorper.
Tailor titles to your ideal customer segment using phrases like "Designed for Busy Professionals
Sed pretium id nibh id sit felis vitae volutpat volutpat adipiscing at sodales neque lectus mi phasellus commodo at elit suspendisse ornare faucibus lectus purus viverra in nec aliquet commodo et sed sed nisi tempor mi pellentesque arcu viverra pretium duis enim vulputate dignissim etiam ultrices vitae neque urna proin nibh diam turpis augue lacus.




