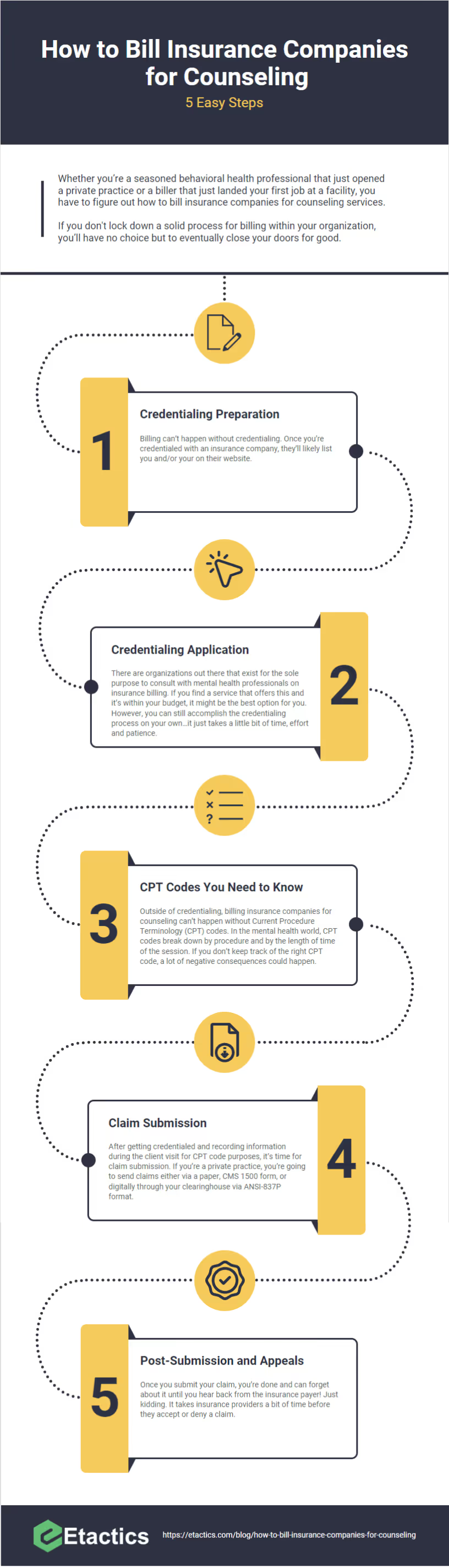
How to Bill Insurance Companies for Counseling: 5 Easy Steps
The majority of mental health professionals’ clients seek your organization for one-on-one or group counseling sessions. Thus, your billing process shouldn’t be on a global level. Instead, all you need to do is figure out how to bill insurance companies for counseling. That’s exactly what this blog post covers.

Whether you’re a seasoned behavioral health professional that just opened a private practice or a biller that just landed your first job at a facility, you have to figure out how to bill insurance companies for counseling services.
Unfortunately, caring for clients is only half of the responsibilities you have on your plate. The other half is dealing with and reporting to insurance companies so that you get paid for your services.
If you don't lock down a solid process for billing within your organization, you’ll have no choice but to eventually close your doors for good.
So the solution to what I’m saying is easy then, right? Come up with a process for billing with your staff, implement it and you can sleep well at night assuming that all your organization’s revenue is in good shape.
It’s not that easy.

Two statistics help paint the dismal picture that is billing insurance companies.
First, 80% of medical bills contain errors. In other words, even if you spend weeks with your team perfecting the billing process for your organization, the industry averages aren’t on your side.
Second, insurance claim denial rates are well over 11%. So, even if there aren’t any errors on the medical bills you send to your patients, their insurance companies still might not compensate you on the back end.
I’d wager to guess that the last thing you thought you would have to worry about when you entered the mental health field was collecting compensation. The reason why you joined this industry in the first place was to help treat your clients, not devote yourself to pleading with insurance organizations to pay what they owe.
To pile on, statistics show that the rates of major depression in adults increased by 61% in less than ten years. Although that means that more clients require your services, it also means that you need to get a handle on your billing processes sooner rather than later.
Yes, I’ve painted a grim picture. But there’s still hope.
You see, the majority of your clients seek your organization for one-on-one or group counseling sessions.
In other words, you likely don’t have to worry about establishing a billing process for more than a handful of different services.
Thus, your process shouldn’t be on a global level. Instead, all you need to do is figure out how to bill insurance companies for counseling. That’s exactly what this blog post covers.
Step 1: Credentialing Preparation
I get it, insurance billing seems like an intimidating process. All of the statistics I threw out in the beginning probably didn’t help ease how you feel about it either. You can do it, but the hardest part is knowing where to start.
Billing can’t happen without credentialing.
Basically, insurance companies came up with the process of credentialing to ensure that you’re qualified for their panels. To put it more simply, they want to make sure that they can trust you.
Once you’re credentialed with an insurance company, they’ll likely list you and/or your on their website.
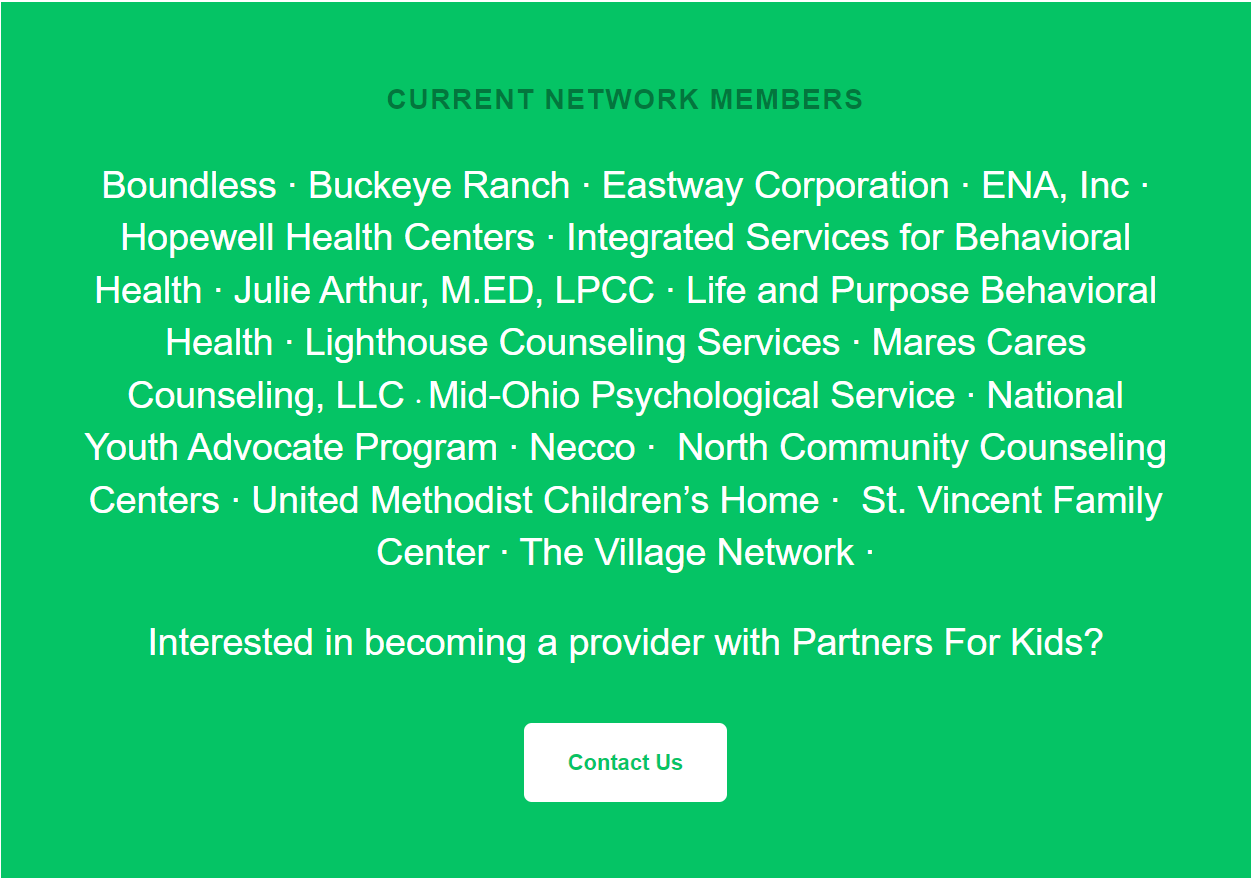
The image above is an example of the list of credentialed mental health organizations with Partners for Kids.
Customers of Partners for Kids that want to schedule a behavioral health appointment would likely visit the webpage that lists credentialed providers and reach out to them. The providers listed by Partners for Kids are “in-network”. That way, Partners for Kids covers the appointment that they need.
If you aren’t credentialed with Partners for Kids in this example, you can likely bill them as an “out-of-network” provider. But there’s a risk associated with doing that because it’s not guaranteed that Partners for Kids would accept it. It depends on whether or not Partners for Kids’ patient policy allows for payment to “out-of-network” providers.
There’s a chance that Partners for Kids does accept that instance, but it’s worth mentioning that government insurance providers don’t. Thus, if you’re not credentialed with Medicare, Medicaid and Tricare, the claims you submit to any of those providers will result in an automatic denial.
Although each insurance’s credentialing process is different, there are preliminary steps you should take to ensure that you’re prepared before the specifics…
- Acquire a tax ID for your organization that’s separate from your SSN
- Seek and obtain malpractice insurance (use the separate tax ID received in step 1)
- Obtain a National Provider Identification (NPI) number
- Ensure that you’re licensed in the state you’re providing service
- Understand your NUCC grouping
- If you’re going to be a Medicare or Medicaid provider, look up and know your taxonomy code
- Apply for a DEA Number if you plan on prescribing clients
- Finalize the location and address of your private practice (PO Box # address suffice)
- Familiarize yourself with CAQH.org and create an account
- Conduct research and make a list of insurance organizations

The preliminary process that I just provided is essentially all of the information that’s required for your CAQH application. You see, CAQH is so important because it’s an industry-accepted database that many insurance companies use as their credentialing database.
Of course, once you create a user and submit it to the CAQH database, you need to keep the information updated. It’s especially important to ensure that you update the information within this database when your license and/or malpractice insurance renews every year.
Step 2: Credentialing Application
Of course, all of the preliminary steps I discussed in the previous section and will discuss in this one don't have to fall on you. There are organizations out there that exist for the sole purpose to consult with mental health professionals on insurance billing. Naturally, there’s a fee associated with utilizing these types of services.
If you find a service that offers this and it’s within your budget, it might be the best option for you. However, you can still accomplish the credentialing process on your own…it just takes a little bit of time, effort and patience.
If you accomplished all of the supplemental steps associated with Step 1 of this blog post, you have a list of providers that you want to get credentialed with. Now, it’s a matter of executing that process itself.
It’s important to note that if you worked at a large facility and you’re starting your private practice, you’re no longer credentialed with those same insurance organizations. In that case, the large facility likely included you under their contract.
Anyway, the application and contracting phase of the insurance credentialing process looks like this…
- Before contacting any organization, determine whether you’re credentialing as a group or as an individual
- If you have multiple locations, have the addresses ready to provide
- Contact each of the insurance companies on your list and ask for their provider relations department
- Ask the provider relations department for a credentialing application
- Review the credentialing application before signing
- Understand documentation and claim submission requirements, appeals processes, reimbursable diagnosis codes, modifier codes and timely filing limits
- Once signed, keep a record of the contract in a safe place
- Once credentialed, the insurance organization will give you access to the provider portion of its website
- Visit that website, create a login and familiarize yourself with the website
- Add all of the contact information to the master list you created in Step 1 of this blog
Although I’ve only listed 9 steps to the credentialing process, it’s important to understand that you can’t finish it in a day. In some cases this process could take months depending on the organization you’re working with. I haven’t even mentioned the fact that some require that you have at least three years of licensure before accepting your application.
You’re also bound to run into the scenario where an insurance company you’re trying to credential with isn’t accepting new providers at the moment. If you run into this situation, retry every six months until there’s availability.
You can see how this process can bring your momentum to a complete stop. The persistence required, though, will pay off in the long run so that you won’t have to worry as much about unnecessary claim denials.
Step 3: CPT Codes You Need to Know
Once you’re credentialed with an insurance organization and you're on its panel, you’ll receive detailed billing information and requirements. You need to keep these requirements in mind for every client session that you provide.
Outside of credentialing, billing insurance companies for counseling can’t happen without Current Procedure Terminology (CPT) codes.
In the mental health world, CPT codes break down by procedure and by the length of time of the session.

For counseling, there are a handful of CPT codes you’ll most commonly use…
- 90791: Exclusive to the first appointment held with a client
- 90832: 16 - 37 minute session
- 90834: 38-52 minute session
- 90837: 53+ minute session
- 90847: 50-minute family psychotherapy when the primary client is present
- 90849: Multiple-family group psychotherapy
- 90853: Group psychotherapy
- 96132: Neuropsychological testing services
It isn’t out of the ordinary for insurance organizations to include CPT codes in billing guides. Unfortunately, though, the codes provided within these guides might not be up-to-date. Since this happens, it’s best to ensure that you have the current CPT manual provided by the American Medical Association.
If you don’t keep track of the right CPT code, a lot of negative consequences could happen. First, it leads to delays in payment. Second, the insurance organization may audit you. Finally, the insurance organization might remove you from its panel.
Step 4: Claim Submission
After getting credentialed and recording information during the client visit for CPT code purposes, it’s time for claim submission.
If you’re a private practice, you’re going to send claims either via a paper, CMS 1500 form, or digitally through your clearinghouse via ANSI-837P format.
Most modern insurance organizations don’t accept paper forms anymore. As such, that’s why you’ll need a secure, digital means to send them. That’s where your clearinghouse partner comes into play.
Anyway, the process of submitting a claim manually also requires persistence…
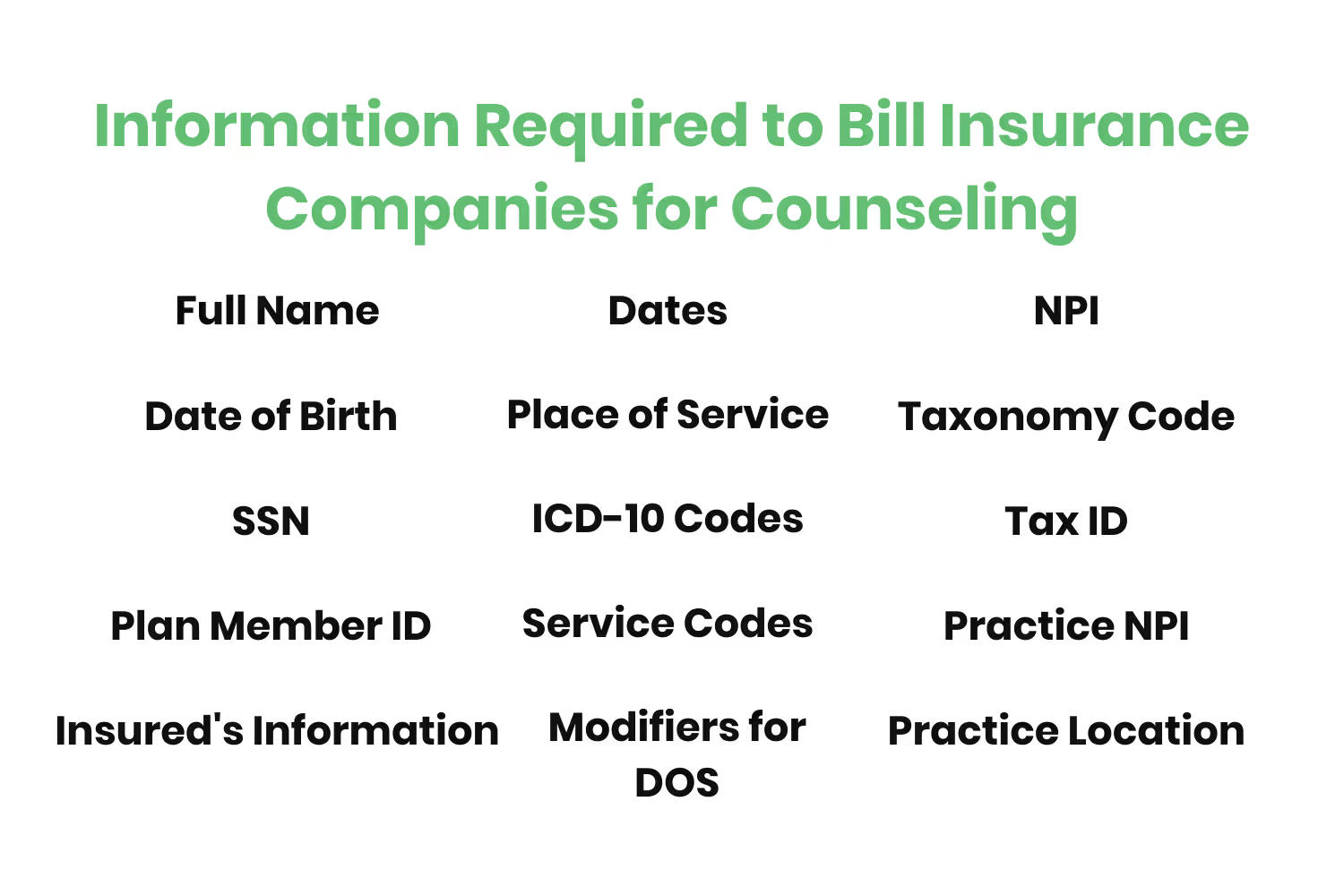
Information Required to Bill Insurance Companies for Counseling
First, you need accurate client information that includes their…
- Full name
- Date of birth
- SSN (if required)
- Plan member ID
- Insured’s information (for dependents)
- Dates
- Place of Service
- ICD-10 Codes
- Service Codes
- Modifiers for each date of service
- Your NPI
- Your Taxonomy Code
- Your Practice Tax ID
- Your Practice NPI
- Your Practice location
Claim Submission process
Once you have all of the information you need, you’re ready to start the submission process. However, it changes based on the technique you rely on.
For a more detailed explanation of billing in the mental health space, check out our definitive guide.
- If you’re using paper (consider going paperless), enter the required information into the CMS-1500 form and mail it to the patient’s payer.
- If you’re manually sending claims via payer portals, log in, follow the screen prompts and type in the information required.
- If you’re using a clearinghouse, submit the claim to the clearinghouse first to pass rejection rules. Once passed, submit the claim to the payer that the clearinghouse is already connected with.
- If your PM system is already integrated with a clearinghouse, click the “submit claim” button.
If your clearinghouse rejects the claim…
- Fix all errors provided within the rejection notice
- Enter missing information
- Have the clearinghouse scan for errors again before payer-level submission
Understand those pesky timely filing limits.
- If you don’t submit your claims within the deadline that the insurance payer details as their timely filing limit, it’s an instant denial.
- Avoid timely filing limit denials by submitting claims regularly
- Create an internal process with defined deadlines
Don’t assume anything.
- Insurance organizations aren’t going to cut you any slack. They have to abide by strict claims processing standards.
- They won’t overlook something incorrect or missing, even if the rest of the information provided is accurate.
- They deal with millions of claims every day so they have to enforce a strict timely filing limit window.
- Don’t take denials personally, learn from them to enhance your business and appeal them.
Follow through.
- The last thing you want to have happen is forget to click the “send” button.
- Many systems allow you to save your claim submission progress.
- If you decide to work through all of your claims and submit them in bulk, don’t forget to click “send”
- If you mail in paper claims, ensure that your clearinghouse has automated logic in place to do this step for you.
Step 5: Post-Submission and Appeals
Claim Status
Once you submit your claim, you’re done and can forget about it until you hear back from the insurance payer! Just kidding.
It takes insurance providers a bit of time before they accept or deny a claim.
Once accepted, the insurance organization will either send you a check via mail or through an electronic funds transfer (EFT) for the claim.

Of course, if payment comes via an EFT, it will just appear in your organization’s bank account with no real explanation. So, how do you keep track of the claims that got accepted and resulted in payment from the insurance provider? Claim status.
Your clearinghouse (or PM system if it’s integrated) should have the ability to provide you with real-time updates as to the status of your claims.
Thus, checking the status of what you submitted and having historical data about your claims should happen regularly.
Appealing Denied Claim
Unfortunately, the payers you submit your claims to aren’t always going to accept everything.
When they don’t accept your submission, it’s called a denial. You don’t receive any payment on denied claims.
However, insurance organizations allow you to resubmit denials. Appealing is the accepted term for the process of fixing errors within denials and resubmitting them.
The appealing process should also exist within your clearinghouse. It should be able to provide you with the denial reason codes and point out exactly where errors within your claims exist.
Conclusion
Billing insurance companies for counseling is the same process as the one used across the entire mental health industry.
The only thing that changes throughout is the patient information, CPT code used, insurance organization you’re submitting claims to and its submission requirements.
I know what you’re thinking, “He practically just identified everything. So, basically, everything about billing changes for every patient, every time?”
Yes, there are a lot of details that change. However, your clearinghouse is there to help get you through the intricacies involved with billing insurance companies every step of the way.
Emphasize your product's unique features or benefits to differentiate it from competitors
In nec dictum adipiscing pharetra enim etiam scelerisque dolor purus ipsum egestas cursus vulputate arcu egestas ut eu sed mollis consectetur mattis pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus mauris aliquam ornare nisl purus at ipsum nulla accumsan consectetur vestibulum suspendisse aliquam condimentum scelerisque lacinia pellentesque vestibulum condimentum turpis ligula pharetra dictum sapien facilisis sapien at sagittis et cursus congue.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Incorporate statistics or specific numbers to highlight the effectiveness or popularity of your offering
Convallis pellentesque ullamcorper sapien sed tristique fermentum proin amet quam tincidunt feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.

Use time-sensitive language to encourage immediate action, such as "Limited Time Offer
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Address customer pain points directly by showing how your product solves their problems
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Vel etiam vel amet aenean eget in habitasse nunc duis tellus sem turpis risus aliquam ac volutpat tellus eu faucibus ullamcorper.
Tailor titles to your ideal customer segment using phrases like "Designed for Busy Professionals
Sed pretium id nibh id sit felis vitae volutpat volutpat adipiscing at sodales neque lectus mi phasellus commodo at elit suspendisse ornare faucibus lectus purus viverra in nec aliquet commodo et sed sed nisi tempor mi pellentesque arcu viverra pretium duis enim vulputate dignissim etiam ultrices vitae neque urna proin nibh diam turpis augue lacus.




